what is the lissauer tract?
- carries pain fibres (which then go to spinothalamic tract)
-contains branches of primary nocireceptors afferents a delta and c fibres
-contains branches of primary nocireceptors afferents a delta and c fibres
what does dolls eyes negative man
If dolls eyes are intact, they stay fixed on a point while moving the head. If dolls eyes are absend they move with head
called the oculocepahlic or vestibuloocular reflex, when retina focuses on a place
called the oculocepahlic or vestibuloocular reflex, when retina focuses on a place
listt he brain stem functions 7
Arousal/consciousness
Respiratory drive
Maintenance of blood pressure
All motor inputs
All sensory inputs (except olfaction/vision)
Autonomic efferents pass through it
Cranial nerve reflexes easily testable
Respiratory drive
Maintenance of blood pressure
All motor inputs
All sensory inputs (except olfaction/vision)
Autonomic efferents pass through it
Cranial nerve reflexes easily testable
define death
The irreversible loss of the capacity for consciousness combined with the irreversible loss of the capacity to breathe
Frage
pupillar reflex
vestibuloocular reflex
conreal reflex
cough and gag reflex
test for apnea (Disconnection test
Prevent hypoxia which could further damage the brain
Ensure that the PaCO2 builds up to critical level (>6.5 kPa)
Absence of respiratory effort
=
vestibuloocular reflex
conreal reflex
cough and gag reflex
test for apnea (Disconnection test
Prevent hypoxia which could further damage the brain
Ensure that the PaCO2 builds up to critical level (>6.5 kPa)
Absence of respiratory effort
=
what does the sulcus limitants do
sulcus limitans (“limiting groove”) marking the separation of the dorsal alar lamina from the ventral basal lami alar is sensory and basal is motor
with what is the trigeminbal lemniscus analogous?
the spinal trigeminal tract?
the proprioreception?
name the three nuclei of the thalamus
the spinal trigeminal tract?
the proprioreception?
name the three nuclei of the thalamus
with the medial lemniscus, crosses to opposite side and ascends with medial lemsnisucs towards thalamus (vetnral posterior)
spinal trigeminal is analogous with the lissauers tract, tracles with spinithalamic tract to thalamus
supplies mursles of mastication
chief, mesencephalic and spinal, spinal is concerend with pain and temp, senory is concerned with the chiefa and the mesencephalic is concere diwth proprioreception, the only one who has hte nulei inside the barinstem
spinal trigeminal is analogous with the lissauers tract, tracles with spinithalamic tract to thalamus
supplies mursles of mastication
chief, mesencephalic and spinal, spinal is concerend with pain and temp, senory is concerned with the chiefa and the mesencephalic is concere diwth proprioreception, the only one who has hte nulei inside the barinstem
with what nerve does the chorda tympni travel and what kind of fibres does it have?
lingual nerve, faste firbe tot anterior 2 3 of the tongue and thas the para sypm to the sublingual and submanidbular gangion
blood supply of eye?
infraorbital form eyneral catotid
opthalamic form the internal carotid
opthalamic form the internal carotid
how would you correct hyperopia ((weitsiching, heisst eyebla is zu kurz):
myopia?
myopia?
biconvex lens
diverging lens
diverging lens
explain the mechanism of horizontal gaze
paramdeian pontne reticular nuclei sends fibres to same side abducends excitatory and contralaeral abducens inhibiory. the abducens on same side sends inhib to same side oculo and to constralteal excti to oculomotor. so lateral gaze can be perdoed, with lateral and contralateral medial recutrs. is via dhte medial longituional fasciculus.
explain internuclear opthalamoplegia
lesion between 6 and 3 in mlf
lesion on left side for example.
abducens cant send excitatory signal to contralteral cn3 when likes to look to the left, so woudl look to left but medial recuts would not follow. if lok to right, owuld be fine. however, convergence is preseved as it does not need the mlf
lesion on left side for example.
abducens cant send excitatory signal to contralteral cn3 when likes to look to the left, so woudl look to left but medial recuts would not follow. if lok to right, owuld be fine. however, convergence is preseved as it does not need the mlf
what is one and a half syndoreme
lets saz lesion on left mlf and lesion in (so form left abducens excitatory fibres to righ oculuo) and right abducends nerve
so, if i want to look to right, cand llook to right, as my abdcunds does not wokr. the oculomotr medial recuts oon ohter side cnat also lookk to hte right as the abducnes is not wrking so cant send its excitatory signals to the contralateal oculomotr. no eyes oare moving at all if i want to look at right.
if i want to look at left i can with ma abducends on left sdie,but cant with my oculomotrs, as the mslf of the left abducnes does ont work co cant send its excitiaroy fibres to the contralateral medial recuts.
so called one and a hlaf beacuse only half a eye is wokring naly the left abducens.
so, if i want to look to right, cand llook to right, as my abdcunds does not wokr. the oculomotr medial recuts oon ohter side cnat also lookk to hte right as the abducnes is not wrking so cant send its excitatory signals to the contralateal oculomotr. no eyes oare moving at all if i want to look at right.
if i want to look at left i can with ma abducends on left sdie,but cant with my oculomotrs, as the mslf of the left abducnes does ont work co cant send its excitiaroy fibres to the contralateral medial recuts.
so called one and a hlaf beacuse only half a eye is wokring naly the left abducens.
what is dyskinesia? what are the tow sfomrs
abnomral movement
hyperkinesa and hypokiendia
hyperkinesa and hypokiendia
list the hypokinetic forms
what is wrong in huntingiotn
what is hungitonons chorea genetially?
what is wrong in huntingiotn
what is hungitonons chorea genetially?
chorea
athetosis
ballismus
dystonia
tic
enkepahlin patches degenerate, cant inhibit the latral lapidum, so swil inhibit subthalamic nuclie which cnat send its excitiraory firbes to medial pall plus substantia nighta pars reticularis, so cant send inhibtors signal tto thalamus. thalams is disnibtied and can send ex to cereblar cotrey so movment is more.
CAG for glumate,k coded 9 to 35 repetition, in ungitontgs more, is is autosomal dominants and is on 4p 16.3
athetosis
ballismus
dystonia
tic
enkepahlin patches degenerate, cant inhibit the latral lapidum, so swil inhibit subthalamic nuclie which cnat send its excitiraory firbes to medial pall plus substantia nighta pars reticularis, so cant send inhibtors signal tto thalamus. thalams is disnibtied and can send ex to cereblar cotrey so movment is more.
CAG for glumate,k coded 9 to 35 repetition, in ungitontgs more, is is autosomal dominants and is on 4p 16.3
what hapens in parkinsons??
the substanita nigha degenartes, dopamine inout decreases, would nroamly be inhibtiory to eknepaholiin patahces in the striatum but sas not dopamine, not inhobiotry to the enkepahlin. so enkaphlin more now and substance p less. so can inhibit the ltaterla pallidum more, so cant sends it inhibotry singal to the subthalamic nculie, to subthalmac can sends its excitaroy singal to the substantai nighra pars retiuclaris and to the medail pallidum which then caninhibit the thalamus so thalamus cant send its excitoray singal nt the cortey so mocment declines.
list the differnet nuclei involved in the faial nerve andwhat they to.
somatic motor nuelus: lie in faical nerve
somatic sensroy sensroy: goe to the grigeminal ,f orm external ear
visceral motor: from superior salvitaro nuclues parasym to the submanidbular via chorda typmani via the the submanidhbler gangion. and form suerior salvitory via greater petrosal via the pyterzgopalatine gnagin to the lacirmal gland.
sensory of mough to to geniculate gangion
viseraosenory: taste form nateior 2 3 of tonhe via chorda typni to the nucleus solitairus
somatic sensroy sensroy: goe to the grigeminal ,f orm external ear
visceral motor: from superior salvitaro nuclues parasym to the submanidbular via chorda typmani via the the submanidhbler gangion. and form suerior salvitory via greater petrosal via the pyterzgopalatine gnagin to the lacirmal gland.
sensory of mough to to geniculate gangion
viseraosenory: taste form nateior 2 3 of tonhe via chorda typni to the nucleus solitairus
what does the sulcus limitants do
sulcus limitans (“limiting groove”) marking the separation of the dorsal alar lamina from the ventral basal lami alar is sensory and basal is motor
what fibres come form the the muscle psindes to the cord in the know jerk reflec which are the ones that come back?
i a afferent (which aare a tzpe of a fibres) to motor neuron, alpha motor neron back. excitin the extensor muslce.
what is a neurite? what does iftform?
one neurite forms the axon, manz form a dendrite
what is the mytatic reflex?
the mytatic reflec is ia afferent to spional ccord, synapses with alpha motor to eztenros so contracts but also sind inhibiotrz interneuon to antoagonist mucle so that not move. gamma motor neuront back to the msuce spinlde to make the contractle part ontract. in cvtnral part find ia afferent, in next to cetnral part of musle spoinle find the secondearz ending.s.
what is a 1 b afferent
golgi, as opposed to sensing strecht and contracitng in the mytatic reflec, the reverse mytatic golgi senses the strecht and whatns muscle to relax againt o reduce strecht
what are tppe s and large tyoe s?
what are type f and type P
what are type f and type P
inhiboborz sall vesicles
excitatorz on i a afferent terminal
excitatorz on i a afferent terminal
bz what drugs woudl baa me potentiated and blocked bz?
otentiated by diayepam and pentobarbitol
blockez by bicuculline (makes it more active)
uses cl channel
blockez by bicuculline (makes it more active)
uses cl channel
what is acute cervical spinal cord injury?
cetnral cord syndorme
great motor impairment, upper more than lower, bloadder dysfucntion sesnory lss below injurg
ocurs in cervical spondylosis or in hyperextension
great motor impairment, upper more than lower, bloadder dysfucntion sesnory lss below injurg
ocurs in cervical spondylosis or in hyperextension
what is a merkel receptor
responds to what stimlu
responds to what stimlu
mechanoreceptor, slow adapting
receptor resonds to a stustained afferent firing fo, needs constant stimuli to keep it going
receptor resonds to a stustained afferent firing fo, needs constant stimuli to keep it going
what are ruffine and merkels
merkels and ruffine MEKRE MERKEL MELKEL are slow adating recetpors able to mainitng friing over long peirords of time to a constant stimuli
what is ruffini
encapsulated mechanorecetpors
in fermis
resebles gogli organ
responds to a mechanical deformation on skin
firing increases progressivlez as stimulius increases
in fermis
resebles gogli organ
responds to a mechanical deformation on skin
firing increases progressivlez as stimulius increases
what are meissner and panicina
fast adapting mechanoreceptors
responds to vibration
produve respnses to a constant stimul but die quiclz awaz though can mainting firing to a rapidly varying stimuli
responds to vibration
produve respnses to a constant stimul but die quiclz awaz though can mainting firing to a rapidly varying stimuli
fascilaes are in a ?
the whoel enrve is in a
the einyelne nerve fibres are in a ?
the whoel enrve is in a
the einyelne nerve fibres are in a ?
perineurium
epineurium
endoreurium
epineurium
endoreurium
to what does a delta and d responds
dela: to pain and presure
c to pain and temperateutre
c to pain and temperateutre
what is the differnece between an unmyelinted ap and myelinated?
unmyelinated travels down axin contionoulsz as a wave but in the myleiate dkwnon as saltatory conduciton as onlz occur at node of ranvier
what is clarkes colum?
in lamina 7, oriign of the ascending dorsal spinocerebellar tract
receives inout form muscles spindles and tendon organs etx
receives inout form muscles spindles and tendon organs etx
expain the dorsal column pathway
has tow nuclie, medial one is gracilis, lateral in cuneatus in medulla, cuneate nuslies recives form upper and graciale form lower l of body but firbes ascend in their faciculius, like cuneate fasciculu,s until thez find their nucleus in the mduula. where thez cross over.
darge diamter inout nerve fibres ofm a alpha and a beta, *ALTS receives fbres form a delta and c )
ascends ippsilaterally ( in ALT ascneds contralaterally)
seconds order neuorns in
seond order neuorn s in the nuclie in medula
convey ino abotu touch and so.
corss ove rin medulla ad ascend in medila lemnicsus to VP thalamus
then projectto somatosensory cortey
darge diamter inout nerve fibres ofm a alpha and a beta, *ALTS receives fbres form a delta and c )
ascends ippsilaterally ( in ALT ascneds contralaterally)
seconds order neuorns in
seond order neuorn s in the nuclie in medula
convey ino abotu touch and so.
corss ove rin medulla ad ascend in medila lemnicsus to VP thalamus
then projectto somatosensory cortey
explain the spinothalamic pathway
carris info form deep pressure and pain and temperature iva a delat and c birbves
decussate at verntral white commisure at spinal cords at samle evel, ascend and then via medial lemnisuc to htalamus ventral posterior to somatosenroz cortex
decussate at verntral white commisure at spinal cords at samle evel, ascend and then via medial lemnisuc to htalamus ventral posterior to somatosenroz cortex
what kind of fibres does the mocirecetpir use in the cns
substance p lreause at snaptic terminals wehre thez act as neurotransmitters (inhibited bz opiods)
what is peripheral neuropahty
spinal cord hemisection
brainstem or cerebral cortex dayfuntion
spinal cord hemisection
brainstem or cerebral cortex dayfuntion
1 loss of sensaiton in hands and feet, due to the large verves which are there who are metabollicallz higha active so tehse are the ones which are affeted most. cuase is diabetes mellitus.
complete secion of spinal cord reuslt in loos of senstaion and motor jfunciton below the injury, however, in hemisecition, affects onlz the left or ight half. in bown seqared, sesnation losst on same die of injur wereas pain and temparte los on opposideside of injruz
3 contalateral loss of senstation or motr
complete secion of spinal cord reuslt in loos of senstaion and motor jfunciton below the injury, however, in hemisecition, affects onlz the left or ight half. in bown seqared, sesnation losst on same die of injur wereas pain and temparte los on opposideside of injruz
3 contalateral loss of senstation or motr
what are the actions of the outer ,, middle and inner ear?
Outer Ear
Collects sound waves(mechanical)
Middle Ear
concentrates sound waves
Inner Ear
Converts mechanical to electrical energy
VIII Nerve conducts electrical energy to auditory cortex
Collects sound waves(mechanical)
Middle Ear
concentrates sound waves
Inner Ear
Converts mechanical to electrical energy
VIII Nerve conducts electrical energy to auditory cortex
what is the simple free field testing test (whisper test)?
Turn patients head to side (so cannot see examiner's mouth)
Apply tragal rub masking to non-test ear (furthest away)
Whisper at arms length, then increase loudness of voice in increments
Patient to repeat numbers/words
Can hear whisper at arm’s length
– Normal hearing
Can hear normal voice at arm’s length
– mild / moderate loss
Can hear loud voice at arm’s length
- moderate / severe loss
Can only hear loud voice close up
- profound loss
Apply tragal rub masking to non-test ear (furthest away)
Whisper at arms length, then increase loudness of voice in increments
Patient to repeat numbers/words
Can hear whisper at arm’s length
– Normal hearing
Can hear normal voice at arm’s length
– mild / moderate loss
Can hear loud voice at arm’s length
- moderate / severe loss
Can only hear loud voice close up
- profound loss
what does the rinne test measure and what is its iterpretation?
conductive hearing loss.
Normal
Positive Rinne – louder at EAM
AC > BC
Abnormal
Negative Rinne – louder on mastoid process
Positive Rinne – Bilateral SNHL
True Negative Rinne
Conductive Hearing loss
BC > AC
False Negative Rinne
- Severe S/N loss on test side = tone heard on contralateral side
Normal
Positive Rinne – louder at EAM
AC > BC
Abnormal
Negative Rinne – louder on mastoid process
Positive Rinne – Bilateral SNHL
True Negative Rinne
Conductive Hearing loss
BC > AC
False Negative Rinne
- Severe S/N loss on test side = tone heard on contralateral side
what is the webers test?
Purpose:
Conductive vs. SNHL in unilateral losses
How:
Strike fork
Place midline of head
Incisors>Vertex>Forehead
unilateral conductive hearing loss: would hear the tuning fork loudest in the affected ear. T
Detection of sensorineural hearing loss: A patient with a unilateral sensorineural hearing loss would hear the sound louder in the unaffected ear,
Conductive vs. SNHL in unilateral losses
How:
Strike fork
Place midline of head
Incisors>Vertex>Forehead
unilateral conductive hearing loss: would hear the tuning fork loudest in the affected ear. T
Detection of sensorineural hearing loss: A patient with a unilateral sensorineural hearing loss would hear the sound louder in the unaffected ear,
with what is frequency measured?
amplitude?
amplitude?
Frequency (pitch) cf. wavelength
Hz / kHz
Intensity (loudness) cf. amplitude
dB
Hz / kHz
Intensity (loudness) cf. amplitude
dB
hearing is measured by pure tone auditometry.
when a is lower than bc what does that indicate?
what doe it indicate iwth they are both lowerd?
what does it indicate if ther is a gap between ac and bc again, but both are in hgeneral lwoered?
when a is lower than bc what does that indicate?
what doe it indicate iwth they are both lowerd?
what does it indicate if ther is a gap between ac and bc again, but both are in hgeneral lwoered?
conducite dearing loss (outer or middle ear)
senorineural loss
mixed loss
senorineural loss
mixed loss
caloric stimulation is used to diagnose nerve damage. what happends, if you put warm in ear?
what happens if u put cold in ear?
what happens if u put cold in ear?
cold water: rapid, side-to-side eye movements called nystagmus. The eyes should move away from the cold water and slowly back.
warm: eyes should now move towards the warm water then slowly away.
warm: eyes should now move towards the warm water then slowly away.
motion of fluid in vestibuar labyrinth activates hair cells. they signal the vestibular nuclei via cranial nerve 8. it then conveys normtaion via two tracts, name them and what they do.
Lateral vestibulospinal tract: The lateral vestibulospinal tract descends ipsilaterally through the entire spinal cord. It terminates in lamina VII and VIII and is excitatory to motor neurons of paravertebral and proximal limb extensors (antigravity muscles). T
Medial vestibulospinal tract: The medial vestibulospinal tract descents bilaterally in the medial portion of the ventral funiculus in a tract also called the medial longitudinal fasciculus (MLF). This tract extends only to cervical and upper thoracic levels. Yokes CN III, IV, VI in eye movements; controlling head and neck position (movement) and gaze control
Medial vestibulospinal tract: The medial vestibulospinal tract descents bilaterally in the medial portion of the ventral funiculus in a tract also called the medial longitudinal fasciculus (MLF). This tract extends only to cervical and upper thoracic levels. Yokes CN III, IV, VI in eye movements; controlling head and neck position (movement) and gaze control
what does a negative tympanogram indicate?
Peak at < 0dPa
Best movement of drum when no negative pressure in EAM thus middle ear pressure must be < atmospheric
Best movement of drum when no negative pressure in EAM thus middle ear pressure must be < atmospheric
what does a flat tympanogram indicate?
When tymp is flat,
usually means 1 of 3 things:
Artefact
Fluid in ME
Perforation
Look at EAM vol.
If large = perf
If normal = fluid
usually means 1 of 3 things:
Artefact
Fluid in ME
Perforation
Look at EAM vol.
If large = perf
If normal = fluid
if peak at zero but very high, what does that indicate in a tympanogram?
Peak at 0dPa, but unusually high amplitude
? Ossicular disruption
? Ossicular disruption
what does it indicate if ther is a peak at 0 but not much?
Peak at 0dPa, but unusually low amplitude
? Stapes fixation
? Stapes fixation
where can i find brocas area?
what does it do?
wenrickes area?
wat does it do?
what does it do?
wenrickes area?
wat does it do?
inferior frontal gyrusof dominant hemisphere
in frontal lobe
abstract thoughts into speech
important for understandig spoken words
connected to brocas area via arcurate fasciculus
understands cat and can think it
in frontal lobe
abstract thoughts into speech
important for understandig spoken words
connected to brocas area via arcurate fasciculus
understands cat and can think it
what is dysphasia?
what is expressive, receptive dysphasia?
what is expressive, receptive dysphasia?
cerebral distubrance of production, comphrehension of written owrk of languge
expressive: brocas area is affected, know wat a cat is, namley its features, but cant prouce the word cat in their mind. there speech is not fluend but comprehension is intact. it is often accompanied by hemiplegia-
receptive: temporal aobe, speecfh is fluent, but does not make any sense. comprehension is thus bad but speech is fluent. it is often accompnaied by a field defect.
expressive: brocas area is affected, know wat a cat is, namley its features, but cant prouce the word cat in their mind. there speech is not fluend but comprehension is intact. it is often accompanied by hemiplegia-
receptive: temporal aobe, speecfh is fluent, but does not make any sense. comprehension is thus bad but speech is fluent. it is often accompnaied by a field defect.
what is dysarthria?
affects the articulation of speech, it is purely motor with intact mental function. muscle sof articulation os afffected (CN 9)
though what can we assess cerebral dominance? 3 things
hand and foot and eye prefernece
though mri by WADA test, inject sodium amytal into left ICA so put one to sleep and then check for handedness
handedness (95 % are hright hadend, of the 5 percent that are left haded only 60 use the left hand, some have bilateral representation or corssed dysphaia)
though mri by WADA test, inject sodium amytal into left ICA so put one to sleep and then check for handedness
handedness (95 % are hright hadend, of the 5 percent that are left haded only 60 use the left hand, some have bilateral representation or corssed dysphaia)
what are the corrseponding c to hyoid, thyroid and cricoid?
hyoid: 3,4
thyroid: 5,6
cricoid: 6,7
thyroid: 5,6
cricoid: 6,7
define neuropraxia,
axonotmosis
neurotmesis
axonotmosis
neurotmesis
pins and needles in tigh due to nerve stretchin, temporoaliy
nerve gets strechted, axons statches off but pathway still intact, it willg row back eventually
nerve gut
nerve gets strechted, axons statches off but pathway still intact, it willg row back eventually
nerve gut
list the nerve supply of hte pinna- 5
Great Auricular
Auriculotemporal
Lesser Occipital
Auricular branch of Vagus
Tympanic Plexus branch
Auriculotemporal
Lesser Occipital
Auricular branch of Vagus
Tympanic Plexus branch
what does the external auditory canal consists of?
what is the ishtmus?
what is the ishtmus?
Outer 1/3 cartilagenous, medial 2/3 bony
Outer 1/3 has hair, sebaceous glands and ceruminous glands
Medially ends in tympanic membrane
Narrowest part is few mm. from T.M.- called Isthmus
list the lymphatic drainage of the ear
Preauricular nodes
Mastoid nodes
External jugular nodes
Mastoid nodes
External jugular nodes
describe the histology of the tympanic membrane
Thin fibrous membrane
Covered externally with stratified squamous epithelium
Covered internally (on middle ear surface) with low columnar epithelium
Circular, about 1 cm. diameter
Concave
Oblique (55 deg.) to EAM, faces forward & downward
Covered externally with stratified squamous epithelium
Covered internally (on middle ear surface) with low columnar epithelium
Circular, about 1 cm. diameter
Concave
Oblique (55 deg.) to EAM, faces forward & downward
where can i find the middle ear?
by which pharnygeal arches is it formed?
of what does it consits?
by which pharnygeal arches is it formed?
of what does it consits?
Aircontaining cavity in Petrous bone
Formed from 1st & 2nd Pharyngeal Pouch
Blind diverticulum from respiratory mucous membrane of nasopharynx
Consists of Eustachian Tube,Middle ear and Mastoid antrum & air cells
Shape like biconcave lens, narrowest part about 2 mm. wide
Formed from 1st & 2nd Pharyngeal Pouch
Blind diverticulum from respiratory mucous membrane of nasopharynx
Consists of Eustachian Tube,Middle ear and Mastoid antrum & air cells
Shape like biconcave lens, narrowest part about 2 mm. wide
what does the lateral wall of the middel ear consist of?
Largely formed by tympanic membrane
Above tympanic membrane, temporal bone hollowed out to form epitympanic recess
Below level of tympanic membrane is hypotympanum
Above tympanic membrane, temporal bone hollowed out to form epitympanic recess
Below level of tympanic membrane is hypotympanum
by whcih stuff is the medial wall fo the inner ear formed??
what is the round and ovale window?
what do we find above the promonory? what is the processus cochleariformis?
what is the round and ovale window?
what do we find above the promonory? what is the processus cochleariformis?
Formed mainly by bony wall of internal ear
Convexity of medial wall formed by promontory - basal turn of cochlea
Behind & above promontory is oval window (fenestra vestibuli) - covered by footplate of stapes
Behind and below oval window is round window (fenestra cochleae) - covered by fibrous membrane called secondary tympanic membrane
Above promontory is ridge which overlies facial canal
Ant. end of facial canal is processus cochleariformis
Below mucous membrane is tympanic plexus
Convexity of medial wall formed by promontory - basal turn of cochlea
Behind & above promontory is oval window (fenestra vestibuli) - covered by footplate of stapes
Behind and below oval window is round window (fenestra cochleae) - covered by fibrous membrane called secondary tympanic membrane
Above promontory is ridge which overlies facial canal
Ant. end of facial canal is processus cochleariformis
Below mucous membrane is tympanic plexus
explain the roof of the inn er ear.
Tegmen Tympani
Separates middle ear from temporal lobe in middle cranial fossa
Continues forward to form roof of canal for tensor tympani
Separates middle ear from temporal lobe in middle cranial fossa
Continues forward to form roof of canal for tensor tympani
expain the floor of the inner ear.
Thin plate
Separates middle ear cavity from jugular fossa and carotid canal
Between these two the tympanic branch of Glossopharyngeal nerve enters middle ear
Separates middle ear cavity from jugular fossa and carotid canal
Between these two the tympanic branch of Glossopharyngeal nerve enters middle ear
explain the anterior wall of the inner ear.
Two canals - Eustachian tube opening
- canal for tensor tympani
Other openings - exit for chorda tympani
- tympanic artery
- caroticotympanic brnches
by what structures is the ossicle formed?
from what embryological structures are they dereived?
what do theya do`?
from what embryological structures are they dereived?
what do theya do`?
Malleus, Incus and Stapes
Synovial joints
Malleus and Incus - 1st arch
Stapes - 2nd arch
Transmit vibrations of tympanic membrane to internal ear
Synovial joints
Malleus and Incus - 1st arch
Stapes - 2nd arch
Transmit vibrations of tympanic membrane to internal ear
what function do the inner ear muscle have =? 2
what muscles are ther (2)
what muscles are ther (2)
Protective function
Damp down over-vibrations caused by loud sounds or low-pitched sound waves
Tensor Tympani - 1st arch (Mandibular N.), tendon curves round processus cochleariformis and inserts into upper part of handle of malleus medially
Stapedius - 2nd arch (Facial N.), tendon emerges from pyramid and inserts into neck of stapes
Damp down over-vibrations caused by loud sounds or low-pitched sound waves
Tensor Tympani - 1st arch (Mandibular N.), tendon curves round processus cochleariformis and inserts into upper part of handle of malleus medially
Stapedius - 2nd arch (Facial N.), tendon emerges from pyramid and inserts into neck of stapes
classification head injrutz
moderate
mild
severe
moderate
mild
severe
moderate is 9 12
severe is 3 8
mild is 13 15
glasgow coma scle
severe is 3 8
mild is 13 15
glasgow coma scle
what odes a diffuse axonal injury inicate
persistante vegetative state due to white matter inrjurz i s NOT brain stem death
what does the cerebellum do
mannanve of balance
contorl of posture and movement
cooordiaation of movement
contorl of posture and movement
cooordiaation of movement
are the purinje fibres of the cerebellar cortex inhibitor of excitiarotz
inhibtiroz aoutput o the cerebellum, onalz putput , use gaba
explain the vestibulocerebellum
whaat is the vestibulospinal tract
whaat is the vestibulospinal tract
equiliblurm
known as achiberebellum
inut from vestibulocohler nerve to to cortex of floccunodular lobe, form tehre to fastigila nucleus, form there to vestibnular nuclei, and form tehre to contralaterallz to medal and latreal vestiulospianl tract and on contralalteral side to medial vestinulospianl atract. which is influecnes. over the nferior cerebelar peduncle
vestiulostnaltract. is influeced bz vestibulocerebellar tract go to extensor muscles to to mainitan posture and standing .
known as achiberebellum
inut from vestibulocohler nerve to to cortex of floccunodular lobe, form tehre to fastigila nucleus, form there to vestibnular nuclei, and form tehre to contralaterallz to medal and latreal vestiulospianl tract and on contralalteral side to medial vestinulospianl atract. which is influecnes. over the nferior cerebelar peduncle
vestiulostnaltract. is influeced bz vestibulocerebellar tract go to extensor muscles to to mainitan posture and standing .
explain the spinocerebellum
spinocerebleum ialso knwon as paleocereelum. is influeced bz the spinocerebellar tract wich are ascending. influeced posture and contorl of movment, contian vermis and paravermis. passto globose and emboiform and a few to astigial.the ones via fastigial go avain to the vestibular nuceli to vestibulspial tract.
emligofrm and flobose reeive the ascending ones via the inferior cerebllar peduncle form dthe dorsal spinocrebllar and via the superior cerebelar educnle the vetnral spnocerebellar tract. then thez sonase there and go to the contralateral red nucleu and then cros gain so end up at the same side to the ruborspianl tract inw ich they descend, whcih influenes fleors.
emligofrm and flobose reeive the ascending ones via the inferior cerebllar peduncle form dthe dorsal spinocrebllar and via the superior cerebelar educnle the vetnral spnocerebellar tract. then thez sonase there and go to the contralateral red nucleu and then cros gain so end up at the same side to the ruborspianl tract inw ich they descend, whcih influenes fleors.
explain ghte spinocerebellar tracts
doral> composed of nuclues dorsalis aetner the cereballum va the infieor cerebellar peducle and have info form the mdulce spindles, tondon orans and joints and cuntaenosiu mecanorecetors.
ventra> corsses over immedialtz ascends though infiero cerebllar peducnel and then corses gaign though the superior cerebellar peduncel so corses TWICE. in addition to sensor zinpout ofmr the various tyes habe the info torm all descending tracts, like cortioosponal rubrospial reticulospinal and vestiblulostpianl tract.
ventra> corsses over immedialtz ascends though infiero cerebllar peducnel and then corses gaign though the superior cerebellar peduncel so corses TWICE. in addition to sensor zinpout ofmr the various tyes habe the info torm all descending tracts, like cortioosponal rubrospial reticulospinal and vestiblulostpianl tract.
wath si tne neocerebellm or the cerebrocerebellum
inout form the primaro mtor cortez andsuplemetarz motor cortez and to pontine nueluson ipsilatera side then form there via middle cereblar peducle to oppostie side to cerebellum carrizng these info for planing and executing the movments. thez termienate in the ltaeral parte s of the cerebllum and sznapte in the ocrtz, then send out fibres ti the dentate which then sends out fibre via the superior cereblar peducnlte to the vetnhral lateral thalamus , some however giong to the red nucleus. thoem the tahlamsu, tthe fibres go back to the cortex.
receive coritobulbospial, supplementar motor, premotr, poteror parietal cortex
receive coritobulbospial, supplementar motor, premotr, poteror parietal cortex
what happends in spinocerebelar dysfunction?
vestibulocerebllar dysfunciotn?
unilteral
ilateranl
vestibulocerebllar dysfunciotn?
unilteral
ilateranl
dzsdiadochokinesia where radilpz alternatin pronation and supination of the forearm becomes impossible
dzsmetria loss of accurate conrto lf force coupled with mistimimg ccan madisnt as dzsmteria the inabilitz ro reach a tarket
fall on side of lesion, lack of coordiation of msulces
wide ased gait, intention tremor
slurring of speech dzsarthria,
in cooriniatin of bot arms, intention tremor
undstez gait, *cerebllar ataxia)
nzstagmus
in mutile scleris habe the inteion termoer, the dzsatria and the nzstamus whic is the charcors triad.
dzsmetria loss of accurate conrto lf force coupled with mistimimg ccan madisnt as dzsmteria the inabilitz ro reach a tarket
fall on side of lesion, lack of coordiation of msulces
wide ased gait, intention tremor
slurring of speech dzsarthria,
in cooriniatin of bot arms, intention tremor
undstez gait, *cerebllar ataxia)
nzstagmus
in mutile scleris habe the inteion termoer, the dzsatria and the nzstamus whic is the charcors triad.
explain wht is happening in the hippocampus
cortical aferent rach dentate via perforant pathwaz to the granule cell lauyer , axons of these cells are called mossz fibres, synase with pyramideal cells in CA3 curnu amonis then leave the CA3 these firbes leacte the hippo via he fimbira but give off colatteralzs schaffner coll that synaose with pzyramidal cells in CA1 whose axones then leave also viea the fbria
what is long term potention
memorz formd din the schaffner cells of theca 1
manz de[polarisatino leads to that
if that happends, the ndma get acrivated. when gluatmedete and d serine binds on them ca go into bell and bidns with calmoduoin, which then activates caclim calmodulin dependent knase whcih makes more ampa recetpors inot supnase and mkes it bigger , SLO enhacnes gene expresison.
manz de[polarisatino leads to that
if that happends, the ndma get acrivated. when gluatmedete and d serine binds on them ca go into bell and bidns with calmoduoin, which then activates caclim calmodulin dependent knase whcih makes more ampa recetpors inot supnase and mkes it bigger , SLO enhacnes gene expresison.
lsit the nerve supply of the iner cavity ear?
blood supplry?
venour drainage
lymph drainage?
blood supplry?
venour drainage
lymph drainage?
Nerve supply from branches of tympanic plexus to mucosa
Blood supply from branches of ext.carotid mainly with a small branch from internal carotid
Veins drain into pterygoid plexus and sup.petrosal sinus
Lymph drainage into parotid and retropharyngeal nodes
Blood supply from branches of ext.carotid mainly with a small branch from internal carotid
Veins drain into pterygoid plexus and sup.petrosal sinus
Lymph drainage into parotid and retropharyngeal nodes
list the 4 steps of hearing.
Outer Ear
Collects sound waves(mechanical)
Middle Ear
concentrates sound waves
Inner Ear
Converts mechanical to electrical energy
VIII Nerve conducts electrical energy to auditory cortex
Collects sound waves(mechanical)
Middle Ear
concentrates sound waves
Inner Ear
Converts mechanical to electrical energy
VIII Nerve conducts electrical energy to auditory cortex

1 anterior auricular
2 superior auricular
3 occipital belly of occipitofrontalis
4 posterior auricular
5 platysma
6 buccinator
7 risorius
8 depressor anguli oris
9 mentalis
10 depressor labil inferioris
11 obicularis oris
12
zygomaticus major
13 zygomaticus minor
14 levator labil superioris
15 levator labil superioris alaeque nasil
16 nasaris
17 procerus
18 obicularis oculi
19 frontal belly of occipitofrontalis
2 superior auricular
3 occipital belly of occipitofrontalis
4 posterior auricular
5 platysma
6 buccinator
7 risorius
8 depressor anguli oris
9 mentalis
10 depressor labil inferioris
11 obicularis oris
12
zygomaticus major
13 zygomaticus minor
14 levator labil superioris
15 levator labil superioris alaeque nasil
16 nasaris
17 procerus
18 obicularis oculi
19 frontal belly of occipitofrontalis
what is bells palsy? 6
what is the cause? 1
how does the disease progress? 3
what are the four other symptoms of bells palsy?
what is the cause? 1
how does the disease progress? 3
what are the four other symptoms of bells palsy?
-Paralysis of the facial nerve resulting in inability to control facial muscles on the affected side....
-or, idiopathic unilateral facial nerve paralysis
-Conditions that can cause a facial paralysis: brain tumour, stroke, meningitis, and diabetes mellitus.
-If no specific cause identified condition is known as Bell's Palsy.
-Most common acute mononeuropathy (disease involving only one nerve)
-Most common cause of acute facial nerve paralysis.
-No readily identifiable cause for Bell's palsy has been found, some evidence suggests herpes simplex type 1 infection may be responsible.
- Rapid onset of partial or complete palsy (usually within single day)
- Inflammation leads to swelling of the facial nerve.
- Nerve swelling and compression in the narrow facial canal lead to nerve inhibition, damage or death.
-Other symptoms:
-hypersensitivity to sound in the affected ear
-watering of the eye (“crocodile tears”)
-drooling from the mouth on the affected side and impairment of taste
-difficulty closing the eye on the affected side
-or, idiopathic unilateral facial nerve paralysis
-Conditions that can cause a facial paralysis: brain tumour, stroke, meningitis, and diabetes mellitus.
-If no specific cause identified condition is known as Bell's Palsy.
-Most common acute mononeuropathy (disease involving only one nerve)
-Most common cause of acute facial nerve paralysis.
-No readily identifiable cause for Bell's palsy has been found, some evidence suggests herpes simplex type 1 infection may be responsible.
- Rapid onset of partial or complete palsy (usually within single day)
- Inflammation leads to swelling of the facial nerve.
- Nerve swelling and compression in the narrow facial canal lead to nerve inhibition, damage or death.
-Other symptoms:
-hypersensitivity to sound in the affected ear
-watering of the eye (“crocodile tears”)
-drooling from the mouth on the affected side and impairment of taste
-difficulty closing the eye on the affected side
what muslces does the posterir auricular branch supply? 2
what muscles does the temporal branch supplz? 3
what musles oes the zygomatic branch supplz? 1
what muscles does the temporal branch supplz? 3
what musles oes the zygomatic branch supplz? 1
Posterior auricular branch
Occipital belly of occipitofrontalis
Posterior auricular muscle of ear
Temporal branch
Frontal belly of occipitofrontalis
Orbicularis oculi (superior part)
Corrugator supercillii
Zygomatic branch
Orbicularis oculi (inferior part)
Occipital belly of occipitofrontalis
Posterior auricular muscle of ear
Temporal branch
Frontal belly of occipitofrontalis
Orbicularis oculi (superior part)
Corrugator supercillii
Zygomatic branch
Orbicularis oculi (inferior part)
what musles does the buccal branch supplz? 9
a. Nasalis
b. Levator labii superioris alaeque nasi
c. Orbicularis oris
d. Levator labii superioris
e. Zygomaticus major
f. Buccinator
g. Zygomaticus minor
h.Levator anguli oris
i. Risorius
b. Levator labii superioris alaeque nasi
c. Orbicularis oris
d. Levator labii superioris
e. Zygomaticus major
f. Buccinator
g. Zygomaticus minor
h.Levator anguli oris
i. Risorius
what muscle does the maginal mandibular branch 3 and cervical branch supplz 1 ?
5. Marginal Mandibular branch
a. Depressor anguli oris
b. Mentalis
c. Depressor labii inferioris
6. Cervical branch
a. Platysma
a. Depressor anguli oris
b. Mentalis
c. Depressor labii inferioris
6. Cervical branch
a. Platysma
what are the four components of the facial nerve?
what to they supply?
what to they supply?
4 components:
Somatic motor (somatovisceral) in pons (muscles of facial expression)
Visceral motor (visceromotor) in medulla (parasympathetic efferent fibres from facial nerve (away form) pregangionic fibres originate in superior salivatory nucleus (located in pontine tegmettum) causes lacrimation and salivation )
Somatic sensory in medula (sensation around ear, goes to trigeminal nucleus receives the somatic sensory input form 7, 9 and 10)
Visceral sensory in medulla (taste to anterior 2/3 of tongue, its nucleus is situated in nuvleus solitarius in medulla, floor of mouth and palate)
Somatic motor (somatovisceral) in pons (muscles of facial expression)
Visceral motor (visceromotor) in medulla (parasympathetic efferent fibres from facial nerve (away form) pregangionic fibres originate in superior salivatory nucleus (located in pontine tegmettum) causes lacrimation and salivation )
Somatic sensory in medula (sensation around ear, goes to trigeminal nucleus receives the somatic sensory input form 7, 9 and 10)
Visceral sensory in medulla (taste to anterior 2/3 of tongue, its nucleus is situated in nuvleus solitarius in medulla, floor of mouth and palate)
from whch pahryngeal arch does the facial nerve arise?
how does the course of it looks like?
what fibres does it carry?
how does the course of it looks like?
what fibres does it carry?
second pharyngeal arch
longest bony course of all cranial nerves, tortuous path
motor, but has some parasym and sensory firbes
longest bony course of all cranial nerves, tortuous path
motor, but has some parasym and sensory firbes
explain the course of the facial nerve in twelv points
1 arises at the pontomedullary junction next to vestibulocolchlear (lateral to abducens) with a large motor root (media) and a smaller sensory (lateral , nervus intermedius)
2 it loops around abducens nuclesu in forth ventricle (loop called internal genu)
- internal genu creates facial colliculus (as it loops aroudn abducends, an elevation in the floor of the 4th venticlue, lesion here results in facial paralysis)
3 exits posterior cranial fossa through internal acoustic meatus
4 facial nerve and accompanying intermediate nerve pass though facial canal and there fuse to form the facial nerve proper
5 nerve enlarge sto become genniculate ganglion (contains cell bodies of sensory affernt neurons)
6 nerve continues through canal and gives off a branch to stapedius and chroda tympani (corda tympanie carries ribres to anterior 2/3 of tongue and pregangionic fibres destined for submandibular region
7 exits skull thoughj stylomastoid foramen
8 gives off posterior auricular nerve as it eremges from stylomastoid foramen (passes posterosuperiorlz to auricle of ear to supplz posterior ausicular muscle and occipital bely of occipitofrontalis)
9 gives off branch to posterior belly of digastric muslce and stylohyoid
10 enters parotid gland
11 devies into upper temporofacial and lower cervicofacial branches
12 facial nerve terminates as 5 branches, temporal zygomatic, marginal mandibular and cervical branches wich supply muscles of facial expression
2 it loops around abducens nuclesu in forth ventricle (loop called internal genu)
- internal genu creates facial colliculus (as it loops aroudn abducends, an elevation in the floor of the 4th venticlue, lesion here results in facial paralysis)
3 exits posterior cranial fossa through internal acoustic meatus
4 facial nerve and accompanying intermediate nerve pass though facial canal and there fuse to form the facial nerve proper
5 nerve enlarge sto become genniculate ganglion (contains cell bodies of sensory affernt neurons)
6 nerve continues through canal and gives off a branch to stapedius and chroda tympani (corda tympanie carries ribres to anterior 2/3 of tongue and pregangionic fibres destined for submandibular region
7 exits skull thoughj stylomastoid foramen
8 gives off posterior auricular nerve as it eremges from stylomastoid foramen (passes posterosuperiorlz to auricle of ear to supplz posterior ausicular muscle and occipital bely of occipitofrontalis)
9 gives off branch to posterior belly of digastric muslce and stylohyoid
10 enters parotid gland
11 devies into upper temporofacial and lower cervicofacial branches
12 facial nerve terminates as 5 branches, temporal zygomatic, marginal mandibular and cervical branches wich supply muscles of facial expression
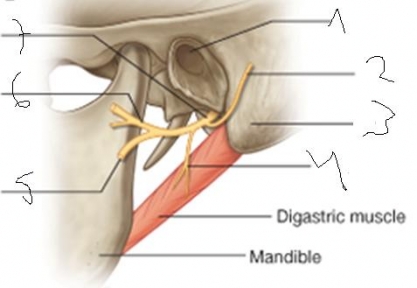
1 external acoutic meatus
2 posteror auricular branch
3 mastoir process
4 digastic branch ( pstoeror belly of digastic muslce)
5 cervicofacial nerve
6 temporofacial nerve
7 facial nerve
2 posteror auricular branch
3 mastoir process
4 digastic branch ( pstoeror belly of digastic muslce)
5 cervicofacial nerve
6 temporofacial nerve
7 facial nerve

1 temporofacial
2 posterior auricular branch
3 cervicofacial
4 parotid gland]
5 cervical branch
6 marginal mandibular branch
7 buccal branch
8 zugomatic branch
9 temporal branch
2 posterior auricular branch
3 cervicofacial
4 parotid gland]
5 cervical branch
6 marginal mandibular branch
7 buccal branch
8 zugomatic branch
9 temporal branch
what is the sensory part of the facial part and where does it arise?
where does the motor nerve arise form the facial nerve?
what is the nervus intermedius destined for wthich two structures via what nerves?
what kind of fibres does the NI have?
when does the NI join the facial nerve?
when does the facial canal start and where does it end?
where does the motor nerve arise form the facial nerve?
what is the nervus intermedius destined for wthich two structures via what nerves?
what kind of fibres does the NI have?
when does the NI join the facial nerve?
when does the facial canal start and where does it end?
NI from the nervus intermedius (presynaptic fibres)
motor fibres arise form the facial nerve nucleus (in pons)
pterygopalatine and submandiubular ganglia via the greater petrosal and chorda tympani
supplies secretomotor fibres to glands in eye, mouth and eye and gustatroy fibres to tongue and palate
when it reaches facial canal joins it at geniculate gangion
internal acoustic canal to the stylomastoid forman
motor fibres arise form the facial nerve nucleus (in pons)
pterygopalatine and submandiubular ganglia via the greater petrosal and chorda tympani
supplies secretomotor fibres to glands in eye, mouth and eye and gustatroy fibres to tongue and palate
when it reaches facial canal joins it at geniculate gangion
internal acoustic canal to the stylomastoid forman
though wich structre does the chorda tympani travel?
it joins with whcih nerve?
after it joined with that nerve to which ganglia does it travel ?
pregangionic parasympathetic fibres of the chorda tympani synapse with postgangionic fibres wich innervate which two structures?
which does the chorda tympani supply?
it joins with whcih nerve?
after it joined with that nerve to which ganglia does it travel ?
pregangionic parasympathetic fibres of the chorda tympani synapse with postgangionic fibres wich innervate which two structures?
which does the chorda tympani supply?
middle ear, infratemporal fossa
lingual nerve
submandibular gangion
submandicular and sublingual salivary glands
anterior 2/3 of the tongue via lingual nerve (branch of mandibular nerve CN v3)
lingual nerve
submandibular gangion
submandicular and sublingual salivary glands
anterior 2/3 of the tongue via lingual nerve (branch of mandibular nerve CN v3)

name the three klayer of the eyeball
1 iris (controls diamter of pupil)
2 posteriof chamber ( filled with vitreous gloassy body or humor is a jelly like substance, 4/5 of eyeball mostlz water, 1 % hzloric acid, maked it jellz like. 0.01 % colagen in young people)
3 ciliary body
4 sclera
5 vitreous body
6 choroid
7 optic axis
8 visual axis
9 foeva centralis
10 optic nerve
11 retina
12 ora serrata ( margin of retina)
13 lens (suspended from the ciliarz bodz. lens changes shape and provies abilitz to focus on near or distant object. lens and conrea provide refractive error, mostlz conrea)
14 conjunctiva (covered by mucous membane which keeps conrea moist bz secreation of the lacrimal gland and by blinking)
15 cornea
16 anterior cha,ber (filled with aqueous humor (watery fluid)
1utermost lyer is sclera and cornea (non vascularised)
2choroid highly vascularised
3 retina mainlz nervous tissue
2 posteriof chamber ( filled with vitreous gloassy body or humor is a jelly like substance, 4/5 of eyeball mostlz water, 1 % hzloric acid, maked it jellz like. 0.01 % colagen in young people)
3 ciliary body
4 sclera
5 vitreous body
6 choroid
7 optic axis
8 visual axis
9 foeva centralis
10 optic nerve
11 retina
12 ora serrata ( margin of retina)
13 lens (suspended from the ciliarz bodz. lens changes shape and provies abilitz to focus on near or distant object. lens and conrea provide refractive error, mostlz conrea)
14 conjunctiva (covered by mucous membane which keeps conrea moist bz secreation of the lacrimal gland and by blinking)
15 cornea
16 anterior cha,ber (filled with aqueous humor (watery fluid)
1utermost lyer is sclera and cornea (non vascularised)
2choroid highly vascularised
3 retina mainlz nervous tissue
name the blood supplz of the eye
Ophthalmic artery
- supplies all arteries of eye
- Arises from internal carotid artery
- Ophthalmic artery divides into RETINAL and CILIARY system before entering eye
1.Retinal artery
-2 inferior branches, 2 superior branches
- piercesNerve head and retina
2. Posterior Ciliary artery
- forms choridal circulation
-Short posterior ciliary artery - penetrate sclera, divide to fine branches, some go forward to form intrascleral arterial circle of Zinn
-Long posterior ciliary artery branches around eye , enters sclera forward of short branches, enters cilary body, iris - forms major arterial circle of iris
- supplies all arteries of eye
- Arises from internal carotid artery
- Ophthalmic artery divides into RETINAL and CILIARY system before entering eye
1.Retinal artery
-2 inferior branches, 2 superior branches
- piercesNerve head and retina
2. Posterior Ciliary artery
- forms choridal circulation
-Short posterior ciliary artery - penetrate sclera, divide to fine branches, some go forward to form intrascleral arterial circle of Zinn
-Long posterior ciliary artery branches around eye , enters sclera forward of short branches, enters cilary body, iris - forms major arterial circle of iris
name the venous drainage of the eye
Vortex veins - takes blood away from iris, ciliary body and choroidal venous blood
Anterior ciliary veins - blood from scleral plexus and ciliary body
Retinal veins run alongside retinal arteries, join to form central retinal vein, Leaves eye via optic nerve
Anterior ciliary veins - blood from scleral plexus and ciliary body
Retinal veins run alongside retinal arteries, join to form central retinal vein, Leaves eye via optic nerve
by what structure is the aqueous fluid produced in the eye?
by the ciliary process which is pat of the ciliary body
list the back abnd front radius curvature of the eye
by how manz microgram does it grow a day?
how much doe it weigh at 18, how much at 85?
it consits mainlz of what?
what is cataract?
by how manz microgram does it grow a day?
how much doe it weigh at 18, how much at 85?
it consits mainlz of what?
what is cataract?
Flatter on front than back
back radius of curvature 6mm approx.
Front radius of curvature 10mm approx.
Grows by 4.5µg a day
At 18 years lens weighs 140mg
At 85 years lens weighs 255mg
35% protein
Cataracts forms in lens - Nuclear caratact - proteins large, become insoluble
back radius of curvature 6mm approx.
Front radius of curvature 10mm approx.
Grows by 4.5µg a day
At 18 years lens weighs 140mg
At 85 years lens weighs 255mg
35% protein
Cataracts forms in lens - Nuclear caratact - proteins large, become insoluble

there are 10 layers of the retina, name them.
a pigmental epithelium
b photoreceptor layer (the outer and inner segemtns of photoreceptors)
c outer limiting membrane
d outer nuclear layer (consits of rods and cones types of photoreceptors)
e ouyter plexiform layer (synapse with horizontal and bipolar cells (the rods and cones)
f inner nuclear layer (consits of amacirne cells, bipolar and horizontal cells)
g inner plexiform layer (where amacine and bipolar cells synapse with ganglino cells)
h layer of ganlion cells
i layer of optic nerve
j iner limiting membrane
b photoreceptor layer (the outer and inner segemtns of photoreceptors)
c outer limiting membrane
d outer nuclear layer (consits of rods and cones types of photoreceptors)
e ouyter plexiform layer (synapse with horizontal and bipolar cells (the rods and cones)
f inner nuclear layer (consits of amacirne cells, bipolar and horizontal cells)
g inner plexiform layer (where amacine and bipolar cells synapse with ganglino cells)
h layer of ganlion cells
i layer of optic nerve
j iner limiting membrane
what is the macular center of vision?
The macula is an oval-shaped highly pigmented yellow spot near the center of the retina of the human eye. has two or more layers of ganglion cells. Near its center is the fovea, a small pit that contains the largest concentration of cone cells in the eye and is responsible for central vision,.
Because the macula is yellow in colour it absorbs excess blue and ultraviolet light that enter the eye, and acts as a natural sunblock or sunglasses for this area of the retina. Structures in the macula are specialized for high acuity vision. Within the macula are the fovea and foveola which contain a high density of cones (photoreceptors with high acuity).
Because the macula is yellow in colour it absorbs excess blue and ultraviolet light that enter the eye, and acts as a natural sunblock or sunglasses for this area of the retina. Structures in the macula are specialized for high acuity vision. Within the macula are the fovea and foveola which contain a high density of cones (photoreceptors with high acuity).
what is the light sensitive segment of the rods?
what is the difference between the vesicles in rods and cones?
what is the difference between the vesicles in rods and cones?

the outer segment
Those of the rods form a series of closed, flattened vesicles, whereas in the cones they remain open to the extracellular space.
what is rhodopsin?
The photopigment is called rhodopsin. It consists of a transmembrane protein (opsin) complexed with a prosthetic group (retinal).
Opsin - glysoprotien
Retinal vit a derivative - from carotenoid
So do need to eat carrots to see at night! - night blindness can be due to prolonged vit a definiceny
Opsin - glysoprotien
Retinal vit a derivative - from carotenoid
So do need to eat carrots to see at night! - night blindness can be due to prolonged vit a definiceny
explain the cycle of retinal (four steps)
1 In dark cis retinal - bent shape - fits into opsin
2 Absorbs phoron - isomeriation - change in shape - become straight - trans-retinal
Transretinal sperates form opsin - bleaching
3. In dark retinal isomerase converts
trans to cis-retinal
4. Cis-retinal binds to opsin
Regenerates photopigment
2 Absorbs phoron - isomeriation - change in shape - become straight - trans-retinal
Transretinal sperates form opsin - bleaching
3. In dark retinal isomerase converts
trans to cis-retinal
4. Cis-retinal binds to opsin
Regenerates photopigment
explain the ion current in phototransduction
- In the dark, Na channels in the outer segment are open
- There is a net flux of Na into the outer segment and this is removed by exchange for K in the region of the cell body
- Electrical neutrality is maintained by an efflux of K through “leakage” channels
- There is, therefore, a dark current which keeps the cell in a relatively depolarised state.
- The transition from 11-cis to all-trans retinal in the light causes a conformational change in the opsin, which, through a series of biochemical events leads to the closure of the Na channels in the outer segment.
-K continues to leave the cell through the leakage channels, driving the membrane potential towards the equilibrium potential for K (said to be hyperpolarising).
Under the relative depolarisation of the dark-adapted state, there is continuous release of neurotransmitter from the synapses on to the bipolar cells, and this is reduced on hyperpolarisation in the light.
- There is a net flux of Na into the outer segment and this is removed by exchange for K in the region of the cell body
- Electrical neutrality is maintained by an efflux of K through “leakage” channels
- There is, therefore, a dark current which keeps the cell in a relatively depolarised state.
- The transition from 11-cis to all-trans retinal in the light causes a conformational change in the opsin, which, through a series of biochemical events leads to the closure of the Na channels in the outer segment.
-K continues to leave the cell through the leakage channels, driving the membrane potential towards the equilibrium potential for K (said to be hyperpolarising).
Under the relative depolarisation of the dark-adapted state, there is continuous release of neurotransmitter from the synapses on to the bipolar cells, and this is reduced on hyperpolarisation in the light.
why are the three differnet tzpes of cones peaking at differnt wave lengths?
The differences in sensitivity are due to differences in the amino-acid composition of the opsin component of the photopigments.
define:
TRICHROMAT
ANOMALOUS TRICHROMAT
DICHROMAT
PROTANOPE -
DEUTERANOPE -
TRITANOPE
MONOCHROMAT -
ACHROMAT -
TRICHROMAT
ANOMALOUS TRICHROMAT
DICHROMAT
PROTANOPE -
DEUTERANOPE -
TRITANOPE
MONOCHROMAT -
ACHROMAT -
TRICHROMAT - Has all 3 cones present, normal colour vision
ANOMALOUS TRICHROMAT - has all 3 cones, but partial deficency in one
DICHROMAT - Has 2 cone types present, 1 completely absent
PROTANOPE - Lacks l-cones “red”
DEUTERANOPE - Lack m-cones “green”
TRITANOPE - Lacks s-cones “blue” Rare
MONOCHROMAT - Has only 1 cone type
ACHROMAT - No functioning cones,
rods only . sees well at night, but apart form that poor vison
ANOMALOUS TRICHROMAT - has all 3 cones, but partial deficency in one
DICHROMAT - Has 2 cone types present, 1 completely absent
PROTANOPE - Lacks l-cones “red”
DEUTERANOPE - Lack m-cones “green”
TRITANOPE - Lacks s-cones “blue” Rare
MONOCHROMAT - Has only 1 cone type
ACHROMAT - No functioning cones,
rods only . sees well at night, but apart form that poor vison
what is emmetropia
myopia
hyperopia
myopia
hyperopia
Normal vision is known as emmetropia. If the eyeball is too long, a distant object is focused in front of the retina, resulting in myopia, or short-sight, which is corrected using a diverging lens. If the eyeball is too short, near objects are focused behind the retina, resulting in hyperopia (previously known as hypermetropia) or long-sight, which is corrected with a converging lens.
what is presbyopia?
Lens grows thicker/heavier with age
Ciliary muscle unable to change lens
shape to focus
Ciliary muscle unable to change lens
shape to focus
what do we undestand in eye under accomodation?
Ability to increase the convexity of lenses to obtain clear image of near object
Lens enclosed in elastic capsule, suspended by ligaments - zonule of Zinn
Ligaments between the periphery of capsule and cilary body
Can change the curvature of the surface by variation in tension
Lens enclosed in elastic capsule, suspended by ligaments - zonule of Zinn
Ligaments between the periphery of capsule and cilary body
Can change the curvature of the surface by variation in tension

what does the iris and ciliarz body contain?
what is the funciton of the riris
what is the pupillary constricots muslce?
thas is the pupillary dilator muslce?
what happens if the ciliary body contracts?
1 cornea
2 pupillarz constictor muslce
3 posteror chamber
4 pupilarz dilator muscle
5 canal of schlemm
6 ciliarz body and muscle
7 suspensory ligament
8 sclera
9 choroid
10 ora serrata
11 lens
12 vitreous body
The iris and ciliary body are specialised parts of the choroid layer of the eye. They contain smooth muscle fibres under autonomic control
The iris serves to adjust the size of the pupil, through which light is admitted to the eye. Its main function, therefore, is to adapt the eye to variations in the amount of ambient light.
The pupillary constrictor muscle consists of circularly arranged fibres. It is antagonised by the radial fibres of the pupillary dilator muscle.
The lens is attached to the ciliary body by the suspensory ligament. Changes in shape of the lens alter the effective focal length of the eye, allowing sharp images of close or distant objects to be formed on the retina (accommodation). When the ciliary muscles contract, the lens becomes more convex, bringing close objects into focus.
2 pupillarz constictor muslce
3 posteror chamber
4 pupilarz dilator muscle
5 canal of schlemm
6 ciliarz body and muscle
7 suspensory ligament
8 sclera
9 choroid
10 ora serrata
11 lens
12 vitreous body
The iris and ciliary body are specialised parts of the choroid layer of the eye. They contain smooth muscle fibres under autonomic control
The iris serves to adjust the size of the pupil, through which light is admitted to the eye. Its main function, therefore, is to adapt the eye to variations in the amount of ambient light.
The pupillary constrictor muscle consists of circularly arranged fibres. It is antagonised by the radial fibres of the pupillary dilator muscle.
The lens is attached to the ciliary body by the suspensory ligament. Changes in shape of the lens alter the effective focal length of the eye, allowing sharp images of close or distant objects to be formed on the retina (accommodation). When the ciliary muscles contract, the lens becomes more convex, bringing close objects into focus.
in the pupillary light reflex, 4 neuronal pathways are involved, name them.
explain the mechansims of the pupillary light reflex.
explain the mechansims of the pupillary light reflex.
Light Reflex - 4 Neurones
First - connects retinal with pre-tectal nucleus in midbrain
Second - pretectal nucleus to Edinger-Westphal nuclues
Third - E-W to ciliary ganglion
Fourth Ciliary ganglion to innervate sphincter pupillae
The pretectal area of the midbrain receives bilateral input from collaterals of ganglion cell axons, signalling the detection of light by either retina. There is then a bilateral projection to the Edinger-Westphal nuclei that provide preganglionic parasympathetic input to the ciliary ganglia. Form these, postganglionic parasympathetic fibres innervate the pupillary constrictor muscle. both eyes constrict
First - connects retinal with pre-tectal nucleus in midbrain
Second - pretectal nucleus to Edinger-Westphal nuclues
Third - E-W to ciliary ganglion
Fourth Ciliary ganglion to innervate sphincter pupillae
The pretectal area of the midbrain receives bilateral input from collaterals of ganglion cell axons, signalling the detection of light by either retina. There is then a bilateral projection to the Edinger-Westphal nuclei that provide preganglionic parasympathetic input to the ciliary ganglia. Form these, postganglionic parasympathetic fibres innervate the pupillary constrictor muscle. both eyes constrict
by what is the pupillary dilator muslce innervated?
The pupillary dilator muscle is innervated by postganglionic sympathetic fibres from the superior cervical ganglion that reach the eye via the ciliary ganglion
explain the accomodation reflex
The accommodation reflex requires detection of a focused image on the retina, so the cortical visual pathway (lgn to primary visual cortex) is involved. The pretectal area receives an input from the visual cortex, and from there there is a parasympathetic pathway innervating the ciliary muscle, similar to that of the pupillary constrictor. The reflex is antagonised by passive tension in the suspensory ligament, so there is no sympathetic innervation of the ciliary muscle.
list the extraocular muscles and their action.
Medial Rectus - adduction
Lateral Rectus - abduction
Superior rectus - elevation, intorsion and adduction
Inferior rectus - depression, extorsion and adduction
Superior oblique - intorsion, depression and abduction
Inferior oblique - extorsion, elevation and abduction
Lateral Rectus - abduction
Superior rectus - elevation, intorsion and adduction
Inferior rectus - depression, extorsion and adduction
Superior oblique - intorsion, depression and abduction
Inferior oblique - extorsion, elevation and abduction

this diagram depicts the regulation of horizontal gaze. explain how it works.
EBN means excitatory burst neurons
IBN menas inhibitory burst neurons
PPRN means paramedian reticular nucleus
Activity of EBN neurons in the left PPRN excitates the ipsilateral abducent motoneurons supplyin ght lateral rectus muscle, whereas IBN neurons inhibit the corresponding contralateral motoneurons. In addition, excitatory interneurons in the abducens nuclei project contralaterally via the medial longitudinal fasciculus to the opposite oculomotor nuclei, to synapse with motoneurons supplying the medial rectus muscles. The combined effect is to turn the eyes to the left.
there are 5 differnt forms of eye movement. define the following.
smooth pursuit
saccades
vestibulo-ocular reflex
optokinetic
vergence
smooth pursuit
saccades
vestibulo-ocular reflex
optokinetic
vergence
reflex fixation of an object on the fovea
Reponse to small slowly moving target
fixation can be initiated and terminated voluntarily or involuntarily
variable speed (5 - 100° / second) reflexly maintained (involuntary eye movements)
intentional (voluntary eye movements)
reflexive (e.g direction of gaze to source of sound or moving object in peripheral field)
constant speed (800° /second)
Vision is suppressed during saccadic eye movement - Saccadic Omission
Saccades faster - if watching thrown ball following hand movenment use smooth pursuit until ball accelerates then saccades to follow the ball
The vestibulo-ocular reflex (VOR) or oculovestibular reflex is a reflex eye movement that stabilizes images on the retina during head movement by producing an eye movement in the direction opposite to head movement, thus preserving the image on the center of the visual field.
The optokinetic reflex allows the eye to follow objects in motion when the head remains stationary (e.g. observing individual telephone poles on the side of the road as one travels by them in a car). The reflex develops at about 6 months of age. [1]
A vergence is the simultaneous movement of both eyes in opposite directions to obtain or maintain single binocular vision
Reponse to small slowly moving target
fixation can be initiated and terminated voluntarily or involuntarily
variable speed (5 - 100° / second) reflexly maintained (involuntary eye movements)
intentional (voluntary eye movements)
reflexive (e.g direction of gaze to source of sound or moving object in peripheral field)
constant speed (800° /second)
Vision is suppressed during saccadic eye movement - Saccadic Omission
Saccades faster - if watching thrown ball following hand movenment use smooth pursuit until ball accelerates then saccades to follow the ball
The vestibulo-ocular reflex (VOR) or oculovestibular reflex is a reflex eye movement that stabilizes images on the retina during head movement by producing an eye movement in the direction opposite to head movement, thus preserving the image on the center of the visual field.
The optokinetic reflex allows the eye to follow objects in motion when the head remains stationary (e.g. observing individual telephone poles on the side of the road as one travels by them in a car). The reflex develops at about 6 months of age. [1]
A vergence is the simultaneous movement of both eyes in opposite directions to obtain or maintain single binocular vision
define the three forms of opthalamoplegia
nuclear - Lesion involves oculomotion nucleus or cranial nerve
supranuclear - lesion invoves cortex or brainstem gaze centres
internuclear - lesion occurs in MLF, between nuclei of oculomotion
supranuclear - lesion invoves cortex or brainstem gaze centres
internuclear - lesion occurs in MLF, between nuclei of oculomotion
define the three forms of nuclear opthalamoplegia
III nerve palsy
Eye down and out, ptosis, pupil dilation
Common causes - aneurysms, diabetes
IV nerve palsy
Superior Oblique - deficit of depression, intorsion, abduction
Common causes - trauma, vascular, diabetes, congenital
VI nerve palsy
Lateral rectus - deficit in abduction
Common causes - congenital, acquired differs with age
In children - infection, trauma, raised intracranial pressure
Young adults - Multiple sclerosis, trauma, diabetes
Older adults - Vascular, diabetes (the only one ooff all the forms which is on contralalteral side)
Eye down and out, ptosis, pupil dilation
Common causes - aneurysms, diabetes
IV nerve palsy
Superior Oblique - deficit of depression, intorsion, abduction
Common causes - trauma, vascular, diabetes, congenital
VI nerve palsy
Lateral rectus - deficit in abduction
Common causes - congenital, acquired differs with age
In children - infection, trauma, raised intracranial pressure
Young adults - Multiple sclerosis, trauma, diabetes
Older adults - Vascular, diabetes (the only one ooff all the forms which is on contralalteral side)
waht are the other three forms of opthalamoplegia ?
saccadic disorder
smooth pursuit disorder
gaze palsy
saccadic disorder
smooth pursuit disorder
gaze palsy
Saccadic disorders - Interrupts voluntary saccades, reflexive saccades retained
Ocular motor apraxia - congenital, inability to make voluntary horizontal saccades
Smooth Pursuit disorders
Smooth pursuit replaced by series of small saccades
Gaze palsy
Progressive supranuclear palsy
Ocular motor apraxia - congenital, inability to make voluntary horizontal saccades
Smooth Pursuit disorders
Smooth pursuit replaced by series of small saccades
Gaze palsy
Progressive supranuclear palsy
name the two forms of internuclear opthalamoplegia
Internuclear opthalmoplegia
Lesion between III and IV nuclei
bilateral often due to MS, unilateral often vascular
Patient often has diplopia - double vision
Unilateral - disrupt the adducting saccades on ipsilateral side, convergence is preserved as those fibres don’t pass through the MLF
Presence of convergence shows that the nerves and nuclei are intact and lesion in MLF
One and a half syndrome
Leison in MLF and abducens nucleus
Causes - MS,pontine stroke or tumour
One and a half syndrome - lesion invloves MLF and ispliateral abducens nerve
Saccades for adduction and abduction lost in ipsilateral eye and adductiing saccades lost in contralateral eye.
One and a half syndrome as all horizontal saccades lost form one eye and half of them from the other
Lesion between III and IV nuclei
bilateral often due to MS, unilateral often vascular
Patient often has diplopia - double vision
Unilateral - disrupt the adducting saccades on ipsilateral side, convergence is preserved as those fibres don’t pass through the MLF
Presence of convergence shows that the nerves and nuclei are intact and lesion in MLF
One and a half syndrome
Leison in MLF and abducens nucleus
Causes - MS,pontine stroke or tumour
One and a half syndrome - lesion invloves MLF and ispliateral abducens nerve
Saccades for adduction and abduction lost in ipsilateral eye and adductiing saccades lost in contralateral eye.
One and a half syndrome as all horizontal saccades lost form one eye and half of them from the other
how many layers does the lateral geniculate nucleus have?
what kind of fibres does each one habe?
what doe the fibres do?
what kind of fibres does each one habe?
what doe the fibres do?
Six layers -1-6
1 and 2 Magnocellular
3-6 Parvocellular
Layers 1, 4 and 6 receive input from nasal fibres from contralateral eye
Layers 2, 3 and 5 receive input from temporal fibres from ipsilateral eye
Magno - colour blind, high contrast sensitivity, low resolution
Parvo - colour selective, low cs, high resolution
what is monocular blindness?
bitemproal hemianopia
homonymous hemianopia
quadrant anopia
macular sparing
bitemproal hemianopia
homonymous hemianopia
quadrant anopia
macular sparing
Damage to the optic nerve on one side (2) results in monocular blindness.
Damage to the chiasm at the midline (3) results in bitemporal hemianopia (here “temporal” refers to the temporal half of the visual field).
Damage to the optic tract on one side results in homonymous hemianopia (here the lesion is on the right side, so there is blindness of the left halves of the visual fields).
Selective damage to the direct or indirect fibres of the optic radiation on one side results in quadrant anopia.
Finally, damage to the visual cortex results in a homonymous anopia, the extent depending on the extent of the cortical lesion. Here the anterior part of the cortex is damaged, thus sparing the representation of the macula (i.e. the most acute part of the retina, including the fovea).
Damage to the chiasm at the midline (3) results in bitemporal hemianopia (here “temporal” refers to the temporal half of the visual field).
Damage to the optic tract on one side results in homonymous hemianopia (here the lesion is on the right side, so there is blindness of the left halves of the visual fields).
Selective damage to the direct or indirect fibres of the optic radiation on one side results in quadrant anopia.
Finally, damage to the visual cortex results in a homonymous anopia, the extent depending on the extent of the cortical lesion. Here the anterior part of the cortex is damaged, thus sparing the representation of the macula (i.e. the most acute part of the retina, including the fovea).
how is light detected?
what kind of photoreceptors are there?
what kind of photoreceptors are there?
Light is detected by the outer segments of the photoreceptor cells, which synapse with bipolar cells. They, in turn, synapse with ganglion cells. The axons of the ganglion cells leave the retina and project (mostly) to the lateral geniculate nucleus (lgn) of the thalamus. Horizontal integration of information is provided by horizontal and amacrine cells.
There are two main types of photoreceptor: rods, which operate in dim light; and cones, which operate in bright light. Furthermore, there are three types of cone, l, m, s each having somewhat different wavelength (colour) sensitivities.
There are two main types of photoreceptor: rods, which operate in dim light; and cones, which operate in bright light. Furthermore, there are three types of cone, l, m, s each having somewhat different wavelength (colour) sensitivities.
Tags: in turn, Light is detected by the outer segments of the photoreceptor cells, synapse with ganglion cells. The axons of the ganglion cells leave the retina and project (mostly) to the lateral geniculate nucleus (lgn) of the thalamus. Horizontal integration of information is provided by horizontal and amacrine cells., which synapse with bipolar cells. They
Quelle:
Quelle:
how many time s does cleft lip and palate occur?
what impact does it have?
treatment?
what impact does it have?
treatment?
1 in 700, 1 in 2000
emotional impact,
difficulitz in feeding breathing and speaking
surgery is treatment
emotional impact,
difficulitz in feeding breathing and speaking
surgery is treatment
what is first arch syndorme?
what are the two subtypes?
what are the two subtypes?
abnromal development o the components of first pharyngeal arch results in congenital abnormalities on the external ears , mandible and palate
results form insufficient migration of neural crest cells into first arch
treacher collins and pierre robin syndorme
results form insufficient migration of neural crest cells into first arch
treacher collins and pierre robin syndorme
what is treacher collins?
how many times does it occur?
what are its featrues?
how many times does it occur?
what are its featrues?
malar hypoplasia ( underdevelopment of zygomatic bones of face)
mandibular hypoplasia
down slanting palpebral fissures
malformed ears
autosomal dominant trait
1 in 10 000
mandibular hypoplasia
down slanting palpebral fissures
malformed ears
autosomal dominant trait
1 in 10 000
what is pierre robin syndrome?
ypoplasia of mandible leading to posterior displacement of tongue resulting in bilateral cleft palate
defect of external ears
manz cases sporadic some appear to have genetic basis
1 in 8500
defect of external ears
manz cases sporadic some appear to have genetic basis
1 in 8500
what is di geogre syndorme ?
also known as 3rd and 4th pharyngeal pouch syndorme
hypoplasia or absence of the thymus and or parathyroid glands with or without cardiovascular defects, ear abnormalities and micrognathia
susceptibiliy infections
normally micro deletion in the q11.2 region of chromosome 22
1:4000
hypoplasia or absence of the thymus and or parathyroid glands with or without cardiovascular defects, ear abnormalities and micrognathia
susceptibiliy infections
normally micro deletion in the q11.2 region of chromosome 22
1:4000
the brain receives several part types of neurotrasmitter inut. name the three main ones and where they originate.
noradrenergic (locus coeruleus form the midbrain)
dopaminergic (vetnral tegemntal area of midbrain)
serotoninergic form raphe of medulla)
all excite
dopaminergic (vetnral tegemntal area of midbrain)
serotoninergic form raphe of medulla)
all excite
dopamine and noradrenaline are chatecholamines. they use a g protein (metabotropic kind) to transmit their signals. what are the intracellular signalling molecules of:
a1 NA
a2 NA
b1 NA
and what do they increase?
what are the intracellular signallling moles of dopamine=
D1
D2
what do they increase (intracellular levels)?
a1 NA
a2 NA
b1 NA
and what do they increase?
what are the intracellular signallling moles of dopamine=
D1
D2
what do they increase (intracellular levels)?
a1 IP3 increase in Ca
a2 cAMP increase in K (presynaptic)
B1 cAMP increase in K (post)
d1 cAMP increase in K and C (post)
d2 (deacrease in cAMP causes decrease in K and decrease and Ca (post)
a2 cAMP increase in K (presynaptic)
B1 cAMP increase in K (post)
d1 cAMP increase in K and C (post)
d2 (deacrease in cAMP causes decrease in K and decrease and Ca (post)
what vessels are normally hurt in subdural and exctradural haematoma?
what are their main characteristics?
what are their main characteristics?
EDH: meidal meningeal aartery lacerates due to temporal head injury
SDH: bridging veins tear, bad since for that needed big blow
EDH lucid intervals (patients seems ok then deteriorates)
SDH: progresses slowly as veins bleed slowly and cuase transient loos of consciousness, high mortality rate
SDH: bridging veins tear, bad since for that needed big blow
EDH lucid intervals (patients seems ok then deteriorates)
SDH: progresses slowly as veins bleed slowly and cuase transient loos of consciousness, high mortality rate
what is a hemiparesis?
in whcih type of herniation syndorme does it happen?
in whcih type of herniation syndorme does it happen?
muslce weakness on one side of the body contralateally
lesions of corticospinal tract
uncal herniation onto cerebral peduncle
lesions of corticospinal tract
uncal herniation onto cerebral peduncle
name and explain briefly the three main types of herniatoin syndrome:
1) subfalcine
cingulate gyrus herniates under falx cerebri, may interfere with blood vessles
2) uncal, transtentrial
the medial portion of the temporal
lobe (uncus) is forced medially and downward over the
tentorium. There is ipsilateral pupillary dilation. The
uncus is pushed medially into the suprasellar cistern.
3) tonsillar
herniation of cerebellar tonsils though the foramen magnum, medula gets compressed and causes cardiac problems and respiratry arrest
cingulate gyrus herniates under falx cerebri, may interfere with blood vessles
2) uncal, transtentrial
the medial portion of the temporal
lobe (uncus) is forced medially and downward over the
tentorium. There is ipsilateral pupillary dilation. The
uncus is pushed medially into the suprasellar cistern.
3) tonsillar
herniation of cerebellar tonsils though the foramen magnum, medula gets compressed and causes cardiac problems and respiratry arrest
what does the cushings triad comprise and why does it happen?
happens in brain injury
bradycardia ( due to vagal stimulation)
hyertension( due to MAP less than ICP)
respiratory irregularity 8due to compressed brain stem)
bradycardia ( due to vagal stimulation)
hyertension( due to MAP less than ICP)
respiratory irregularity 8due to compressed brain stem)
how can we treat raised intracranial pressure? three possibilities
operate
hyperventialte ( results in a decrease in pa02 which causes vasoconstriction in cranium and thus decreases pressure, may cuase ischemia though
mannitol (can t cross BBB, is similar to glucose (the alcohol in mannose) and acts like a osmotic diuretic: suchs all the water our of brain,;the bad thing is that it looses effectiveness with repeated doeses and can cause renal failure)
hyperventialte ( results in a decrease in pa02 which causes vasoconstriction in cranium and thus decreases pressure, may cuase ischemia though
mannitol (can t cross BBB, is similar to glucose (the alcohol in mannose) and acts like a osmotic diuretic: suchs all the water our of brain,;the bad thing is that it looses effectiveness with repeated doeses and can cause renal failure)
why does a pupil dialte in uncal herniation?
compression of oculomotor nerve causes oculomotor nerve palsy
- ptosis of eyelid (unopposed action of obicularis oculi, paralysis of levator palpebrae superioris)
- fully dialatd eye (unopposed action fo dilator pupillae as parasympathetic output from the oculomotr nerve is damaged which would cuase vasoconstriciton
- fullly abducted and depressed eye due to unopposed aciton fo the lateral rectus and superior oblique, abduction occurs due to alteral rectus, and depression occurs due to superior oblique; paralysed superior rectus and inferior oblique
- ptosis of eyelid (unopposed action of obicularis oculi, paralysis of levator palpebrae superioris)
- fully dialatd eye (unopposed action fo dilator pupillae as parasympathetic output from the oculomotr nerve is damaged which would cuase vasoconstriciton
- fullly abducted and depressed eye due to unopposed aciton fo the lateral rectus and superior oblique, abduction occurs due to alteral rectus, and depression occurs due to superior oblique; paralysed superior rectus and inferior oblique
which muscles are paralysed in oculomotor palsy?
superior rectus (makes upwards movement with inferior oblique)
inferior oblique
medial rectus (inward movement)
inferior rectus (makes downward movement with superior oblique)
levator palpebrae superioris
so unapposed movemnt of lateral rectus (causes outward movement)
unopposed action of suerior oblique and lateral rectus (outward and down)
inferior oblique
medial rectus (inward movement)
inferior rectus (makes downward movement with superior oblique)
levator palpebrae superioris
so unapposed movemnt of lateral rectus (causes outward movement)
unopposed action of suerior oblique and lateral rectus (outward and down)
what does the glasgow coma scale measure?
what are the domains that it covers?
what are the scores you can get?
what are the domains that it covers?
what are the scores you can get?
consciousness
eye opening, verbal response, motor response
eye openiing:
4 - 1
4 sponatneous eye opening
3 to speech open
2 to pain open ( nailbed pressure, supraorbital pressure, sternal rub)
1 none
verbal response
5 orientated
4 confused
3 inappropriate words
2 incomprehensive sounds
1 none
motor response
6 obeys
5 localises ain
4 mormal flexion
3 abnomral flexion
2 extension
1 none
eye opening, verbal response, motor response
eye openiing:
4 - 1
4 sponatneous eye opening
3 to speech open
2 to pain open ( nailbed pressure, supraorbital pressure, sternal rub)
1 none
verbal response
5 orientated
4 confused
3 inappropriate words
2 incomprehensive sounds
1 none
motor response
6 obeys
5 localises ain
4 mormal flexion
3 abnomral flexion
2 extension
1 none
what is the role of CSF? 6
-Maintaining environment of neurones & glia ( provies meansof messenger molecules to glial and neurons)
- Removal of metabolites
- Mechanical cushion between brain and skull
-? Lymphatic system for brain ( brain does not have one but though the csf flow, the bad stuff gets washed away since it is a one way flow)
-Conduit for polypeptide hormones
-pH affects pulmonary ventilation
- Removal of metabolites
- Mechanical cushion between brain and skull
-? Lymphatic system for brain ( brain does not have one but though the csf flow, the bad stuff gets washed away since it is a one way flow)
-Conduit for polypeptide hormones
-pH affects pulmonary ventilation
which structures are passed at lumber puncture?
skin, subcutaneous tissue, fat, supraspinous ligament, interspinous ligament, ligamentum flave (between the laminas), dura, arachnoid

1 anterior communicating artery
2 anterior cerebral artery
3 internal catorid
4 middle cerebral artery
5 posterior communicating
6 superior cerebellar artery
7 pontine arteries
8 basilarartery
9 -
10 anterior spinarl artery
11 osteror inferior cerebellar atery
12 vertebral artery
13 anteror inferior cerebellar artery
14 posterior cerebral artery
15 oculomotor nerve
16 middle cerebral artery
2 anterior cerebral artery
3 internal catorid
4 middle cerebral artery
5 posterior communicating
6 superior cerebellar artery
7 pontine arteries
8 basilarartery
9 -
10 anterior spinarl artery
11 osteror inferior cerebellar atery
12 vertebral artery
13 anteror inferior cerebellar artery
14 posterior cerebral artery
15 oculomotor nerve
16 middle cerebral artery
the cerebral blood flow is normally 50 mls per 100g hoch minus er minute. what happens if it is
25
15
12
10?
25
15
12
10?
eeg becomes flat ( restricted electircal flow)
physiollogic paraöysos
brain stem auditroy evoke responses change (primitive funcitons down)
alterations in cell membrane transport, cell death
physiollogic paraöysos
brain stem auditroy evoke responses change (primitive funcitons down)
alterations in cell membrane transport, cell death
inside head, brain occupies how much percent in ml?
csf?
blood?
what is the pressure in the brain?
what it the presrure in brain a combination of?
csf?
blood?
what is the pressure in the brain?
what it the presrure in brain a combination of?
1400 ml, 80 percent
150 ml 10 percent
150 ml 10 percent
10 - 15 mmHg, above athmospheric in adults
combination of tissue pressue, CSP pressure, arterial pressure pulsation , respiratory pressure
CPP = mean arterila pressure - intracranial pressure
150 ml 10 percent
150 ml 10 percent
10 - 15 mmHg, above athmospheric in adults
combination of tissue pressue, CSP pressure, arterial pressure pulsation , respiratory pressure
CPP = mean arterila pressure - intracranial pressure
what is an eeg?
elctroencephalography
measures the electrical signals of the brain
lower when eyes are closed (the signales) as they are afected by the state of arousal of the cerebral cortex
used o diagnose elpilepsy and brain death
measures the electrical signals of the brain
lower when eyes are closed (the signales) as they are afected by the state of arousal of the cerebral cortex
used o diagnose elpilepsy and brain death
with what do we record electrical signals from contracting muscles?
electromyogram or EMG
what is atls?
management of acute trauma
check the abcde
A - Airway Maintenance with Cervical Spine Protection
B - Breathing and Ventilation
C - Circulation with Hemorrhage Control
D - Disability (Neurologic Evaluation)
E - Exposure / Environmental control
check the abcde
A - Airway Maintenance with Cervical Spine Protection
B - Breathing and Ventilation
C - Circulation with Hemorrhage Control
D - Disability (Neurologic Evaluation)
E - Exposure / Environmental control
terry has a increased respiratory rate after a big accident.. hay might that be?
t2 to t 9 dont work
intercostals are paralysed, has to use accesory muscles
hypoventilation
tachypnea
paraoocical abdominal movementts due to abdominal wall weakness
uses diaphragm to breath
uses up lots of energy due to use of accesory muscles , might result in respiratory failure
intercostals are paralysed, has to use accesory muscles
hypoventilation
tachypnea
paraoocical abdominal movementts due to abdominal wall weakness
uses diaphragm to breath
uses up lots of energy due to use of accesory muscles , might result in respiratory failure
what is neurogenic shock?
what are the signs?
what are the signs?
caused by sudden loss of autonomic nervous system control to smooth muscle and wall due to spinal cord or brain damage
hypotension with high thoracic and cercvical injury
- loss of descending pathways
- vasodilation due to sympathetic loss
- bradycardia due to the loss
- warm and dry extremities
- priapism
- venous pooling
hypotension with high thoracic and cercvical injury
- loss of descending pathways
- vasodilation due to sympathetic loss
- bradycardia due to the loss
- warm and dry extremities
- priapism
- venous pooling
what is spinal shock?
spinal shock is loss of sensation accompanied by motor paralysis with initial loss but gradual recovery of reflexes, following a spinal cord injury (SCI)
descriptive term for fallcid paralysis and loos of reflexes
can develop spastic contraction
descriptive term for fallcid paralysis and loos of reflexes
can develop spastic contraction
what is MRC (muscle power grading)?
grade form zero to five
0 no movement
1 flicker of movment
2 movement iwth gravity eliminated
3 movement against gravity
4 loess than normal power
5 nomral power
0 no movement
1 flicker of movment
2 movement iwth gravity eliminated
3 movement against gravity
4 loess than normal power
5 nomral power
what is a spinal bladder?
initalliy: bladder full not appreciated
bloaader distends dribbeling incontinence
later: bladder spastic, and only holds small volume, hypersensitve
emties suddenly and reflely
flling may stimulate sweating, pallor, flushing, paroxymal hypertension
bloaader distends dribbeling incontinence
later: bladder spastic, and only holds small volume, hypersensitve
emties suddenly and reflely
flling may stimulate sweating, pallor, flushing, paroxymal hypertension
what is priapism?
- reflex reaction
-intact parasympathetic reflex arc at s3 and 3
- loss of sympathetic tone leads to dominance of parasympathetics
-intact parasympathetic reflex arc at s3 and 3
- loss of sympathetic tone leads to dominance of parasympathetics
wha tis bown sequard syndome?
- loss or sensation and mtor function (paralysis and ataxis)
- caused by lateral hemisection of spinal crod
- occurs at same side of spinal infury and loss of pain and temerpature on opposite site
- motor and numbness to touch, vibraction loss on same side
- caused by lateral hemisection of spinal crod
- occurs at same side of spinal infury and loss of pain and temerpature on opposite site
- motor and numbness to touch, vibraction loss on same side
what is central cord syndrome?
- acute cervical spinal cord injury
- great mtor impairment upper limb more than lower limb+
- bladder dysfunction and sensory loss below infury
- occurs in cervical spondylosis if neck hyperextended or in a hyperextensive injury
- great mtor impairment upper limb more than lower limb+
- bladder dysfunction and sensory loss below infury
- occurs in cervical spondylosis if neck hyperextended or in a hyperextensive injury

a alpha motor neuron
b gamma m otor neuron axon
c afferent neuron axons
d secondary endings of afferent fibres (type 2 fibres)
e extrafusal muscle fibres
f primary endings (type 1 a afferent)
g non contractlie central part of intrafusal fibres
h contractile portion of intrafusal fibres
i also contractile part
j intrafusal fibre
k capsule
b gamma m otor neuron axon
c afferent neuron axons
d secondary endings of afferent fibres (type 2 fibres)
e extrafusal muscle fibres
f primary endings (type 1 a afferent)
g non contractlie central part of intrafusal fibres
h contractile portion of intrafusal fibres
i also contractile part
j intrafusal fibre
k capsule
the musle spindle detects change in length and sends sensory information back to the spianl cord. by which two afferent fibres does it do that?
primary endings ( 1a afferent) wrapped around cetnral portion of intrafdusal fibres) detect change in length and speed during strecht
secondary nerve endings (type 2 ) are clustered around the end segments of the fibres and are only sensitive to change in length
secondary nerve endings (type 2 ) are clustered around the end segments of the fibres and are only sensitive to change in length
what deos blood in meningiteis indacte in csf?
increased priten, decrasesglucose, ncreased WBC< polymorphonuclear cvells
what happends i f ml 100 g hoh minus 1 per minute is at
50
25
15
12
10
50
25
15
12
10
50 is mnomral
25 eeg becomes flat
15 phzsiological paralysis
23 brain stem auditorz evoked response change
cell eath, alternd cell emembrane transprot
25 eeg becomes flat
15 phzsiological paralysis
23 brain stem auditorz evoked response change
cell eath, alternd cell emembrane transprot
stroke in posterior prat of visual cotex
bitemporal hemianopia with macuoar spaing
naular area is supplied bz middl meingela artery so spaing
naular area is supplied bz middl meingela artery so spaing
what is the stretch reflex?
how does it function?
how does it function?
negative feedback mechansim to resist pssive change in muslce length. if stretched, then contracts extensor to counteract lenghening which is achieved on tapping the muscle e.g. in jerk reflex wich a little hammer on the patellar tendon (quadriceps femoris)
- 1a afferent senses change
- start to fire ap
- synaoses with alpha motor neuron in ventral horn
- apha motor neuron sends impulse back to extrafusal muscle fibres to contract
- type 2 ribres terminat on interneurons, transmit delayed signals to anteror horn
- 1 a afferent also sends signals to an interneuron (inhibitors) which synapses with motor neuron of flexor muscle (antagonist)
- initiates inhibition of flexor muscle, so movement is only extension
- descending pathways coactivate alpa and gamma neurons, gamma neuron make endportion contract of intrafusal mucle fibre
- so takes slack out of the spindle
- as a reflex pathway, does not involve brain too much, only gets commanding signals
- 1a afferent senses change
- start to fire ap
- synaoses with alpha motor neuron in ventral horn
- apha motor neuron sends impulse back to extrafusal muscle fibres to contract
- type 2 ribres terminat on interneurons, transmit delayed signals to anteror horn
- 1 a afferent also sends signals to an interneuron (inhibitors) which synapses with motor neuron of flexor muscle (antagonist)
- initiates inhibition of flexor muscle, so movement is only extension
- descending pathways coactivate alpa and gamma neurons, gamma neuron make endportion contract of intrafusal mucle fibre
- so takes slack out of the spindle
- as a reflex pathway, does not involve brain too much, only gets commanding signals
what is the inverse mytatic reflex?
- muscles contract (possibly due to the stretch reflex), produce tension at the point where the muscle is connected to the tendon, where the golgi tendon organ is located.
- golgi tendon organ records the change in tension, and the rate of change of the tension
- tension exceeds a certain threshold
- triggers the lengthening reaction which inhibits the muscles from contracting and causes them to relax
- golgi tendon organ helps to protect the muscles, tendons, and ligaments from injury
-lengthening reaction is possible only because the signaling of golgi tendon organ to the spinal cord is powerful enough to overcome the signaling of the muscle spindles telling the muscle to contract.
- golgi tendon organ records the change in tension, and the rate of change of the tension
- tension exceeds a certain threshold
- triggers the lengthening reaction which inhibits the muscles from contracting and causes them to relax
- golgi tendon organ helps to protect the muscles, tendons, and ligaments from injury
-lengthening reaction is possible only because the signaling of golgi tendon organ to the spinal cord is powerful enough to overcome the signaling of the muscle spindles telling the muscle to contract.
what can you say about a neuron?
- highly active and express larger portion of genome than any other cell type
- euchrmatic nucleus wich numerous pores connecting to cytoplasm
- nucleus called karyon
- body or soma called perikaryon
- has nissl granules, are rough er with ribosomes
- euchrmatic nucleus wich numerous pores connecting to cytoplasm
- nucleus called karyon
- body or soma called perikaryon
- has nissl granules, are rough er with ribosomes
the somata of the senory neurons are located in the dorsal root ganglion. name its braches and where they go to.
each senory neuron gives rise to a single process whcih then branches again into a central branch, whcih travels to the spinal cord and a a peripheral branch which trables to the sensory endings of the periphery (e.g. muslce spindle)
what is the flexor reflex?
- painful stimuli elicits it , causing withdrawal
- mediate dby polysynaptic reflex in which interneurons are excited first and then relay signal to motorneuron
- primary afferent pain fibres activate these interneurons in the grey matter, these activate alpha motor neurons that innervate flexor muslce
- flexion of more than one joint is achieved by coordinated action fo more than one spinal segment which is achieved by collateralisaton of primary affernet with interneurons
- mediate dby polysynaptic reflex in which interneurons are excited first and then relay signal to motorneuron
- primary afferent pain fibres activate these interneurons in the grey matter, these activate alpha motor neurons that innervate flexor muslce
- flexion of more than one joint is achieved by coordinated action fo more than one spinal segment which is achieved by collateralisaton of primary affernet with interneurons
what is the flexor and corssed extensor reflex?
-activation of weight bearing limb in flexor reflex causes simultaneously reflex extension of contrallateral limb to take the weight ot the body and thus maintain stable posture
- mediated by axon collateral which corss the midline of the cord and excite alpha motor neurons of contralateral linb extensor muslce and inhibig the flexors
- mediated by axon collateral which corss the midline of the cord and excite alpha motor neurons of contralateral linb extensor muslce and inhibig the flexors
what is the neurotransmitter in motorneural synapses in the cns that is excitory?
glutamate (amino acid=
what is a glutamate receptor?
what are the agonists and antagonists?
what are the agonists and antagonists?
-Glutamate receptors are synaptic receptors located primarily on the membranes of neuronal cells
-Glutamate receptors are responsible for the glutamate-mediated post-synaptic excitation of neural cells
ionotropic agonists (Ligand-gated ion channels (LGICs) are one type of ionotropic receptor or channel-linked receptor. They are a group of transmembrane ion channels that are opened or closed in response to the binding of a chemical messenger such as a neurotransmitter)
- AMPA(kainate) (opens for the n and k channels)
- NMDA(opens for the na k and ca channels)
antagonists
AP5
CNQX
-Glutamate receptors are responsible for the glutamate-mediated post-synaptic excitation of neural cells
ionotropic agonists (Ligand-gated ion channels (LGICs) are one type of ionotropic receptor or channel-linked receptor. They are a group of transmembrane ion channels that are opened or closed in response to the binding of a chemical messenger such as a neurotransmitter)
- AMPA(kainate) (opens for the n and k channels)
- NMDA(opens for the na k and ca channels)
antagonists
AP5
CNQX
what is a renshaw cell?
A type of inhibitory interneuron found in feedback circuits in the central nervous system that control the level of excitation of motor neurons. The Renshaw cells receive input from side branches (collaterals) of motor axons and in turn form inhibitory synapses with the motor-neuron cell bodies.
can synapse with same or different motor neurons
what is gaba?
neurotransmitter used in the cns to inhibit impulses
is formed by decarboxylation of glutamte
binding causes the opening of ion channels to allow the flow of either negatively charged chloride ions into the cell or positively charged potassium ions out of the cell. This action results in a negative change in the transmembrane potential, usually causing hyperpolarization.
thus creats ISPS
is formed by decarboxylation of glutamte
binding causes the opening of ion channels to allow the flow of either negatively charged chloride ions into the cell or positively charged potassium ions out of the cell. This action results in a negative change in the transmembrane potential, usually causing hyperpolarization.
thus creats ISPS
there are two types of muscle spindles. name them
nuclear bags (muslce spindles congregated to bags in central portion)
nuclear chain (have nuclei alinged ina chain)
primary sensroy nerve endings excite both
secondary nerve endings ecxcite only nuclear chain
nuclear chain (have nuclei alinged ina chain)
primary sensroy nerve endings excite both
secondary nerve endings ecxcite only nuclear chain
which effernet fibres supply the extrafusal fibres?
which efferent fibres suply the intrafusal fibres?
which efferent fibres suply the intrafusal fibres?
alpha motor neuron
gamma motor neuron
gamma motor neuron
how to the a delta and c fibres travel?
Neospinothalamic tract
- terminate on the dorsal horn (used to be primary sensory nerves) of the spinal cord (secondary sensory neurons, synapse with them there) where they synapse with the dendrites of the neospinothalamic tract
-travel up the spine to the brain and cross the midline through the anterior white commissure (lamina 10 after grey commisure)
- passing upwards in the contralateral anterolateral columns.
- terminate in thalamus and synapse with the dendrites of the somatosensory cortex
- this pain stimluated by temperature and mechanical
Paleospinothalamic tract
- Slow pain is transmitted via slower type C fibers to laminae II and III of the dorsal horns, together known as the substantia gelatinosa. - Impulses are then transmitted to nerve fibers that terminate in lamina V, also in the dorsal horn, synapsing with neurons that join fibers from the fast pathway, crossing to the opposite side via the anterior white commissure
- traveling upwards through the anterolateral pathway (spinothalamic tract)
- terminate throughout the brain stem, with one tenth of fibres stopping in the thalamus and the rest stopping in the medulla, pons
-Slow pain is stimulated by chemical stimulation,
- terminate on the dorsal horn (used to be primary sensory nerves) of the spinal cord (secondary sensory neurons, synapse with them there) where they synapse with the dendrites of the neospinothalamic tract
-travel up the spine to the brain and cross the midline through the anterior white commissure (lamina 10 after grey commisure)
- passing upwards in the contralateral anterolateral columns.
- terminate in thalamus and synapse with the dendrites of the somatosensory cortex
- this pain stimluated by temperature and mechanical
Paleospinothalamic tract
- Slow pain is transmitted via slower type C fibers to laminae II and III of the dorsal horns, together known as the substantia gelatinosa. - Impulses are then transmitted to nerve fibers that terminate in lamina V, also in the dorsal horn, synapsing with neurons that join fibers from the fast pathway, crossing to the opposite side via the anterior white commissure
- traveling upwards through the anterolateral pathway (spinothalamic tract)
- terminate throughout the brain stem, with one tenth of fibres stopping in the thalamus and the rest stopping in the medulla, pons
-Slow pain is stimulated by chemical stimulation,
what myelin producing insulating cells are there in the cns and pns?
oligodentries (microglia producing myelin)
schwann cells
schwann cells
what is white matter?
what is grey matter?
what is grey matter?
ascending and descendng fibres
cell bodies, itnerneurons, second order neurons, is divided into 10 lamina, 1 to 6is at dorsal horn
cell bodies, itnerneurons, second order neurons, is divided into 10 lamina, 1 to 6is at dorsal horn
where can one find visceral afferents in the laminas in the greay matter?
whre can we find the a delta and c fibres there?
whre can we find the a delta and c fibres there?
lamina 1 to 5
almina 1 and 2
almina 1 and 2
what are thre three components of pain?
Sensory
what it feels like
Affective
emotional element - pain and sport, at rest, under stress or anxiety
Autonomic
effects are common (increased heart rate)
what it feels like
Affective
emotional element - pain and sport, at rest, under stress or anxiety
Autonomic
effects are common (increased heart rate)
in nuerophysiology, what does sensitivity relate to (pain)?
on what depends the spped of conduction?
on what depends the spped of conduction?
sensitivity relates to the proximtiy of resting potential and treshhold potential
degree of myelination
degree of myelination
what are nocireceptors?
Nociceptors are the nerves that
transduce
transmit noxious stimuli from the periphery to the centre
terminate on 2nd order neurones in the dorsal horn
they have their cell bodies in the DRG
transduce
transmit noxious stimuli from the periphery to the centre
terminate on 2nd order neurones in the dorsal horn
they have their cell bodies in the DRG
what are fibre type A delta fibres?
responsible for fast or first pain
sense pain and temperature
activated by noxious mechanical and heat stimuli
Transmit sharp pain following injury
can be subdivided
- low threshold hence respond quickly in normal circumstances but rapidly adapt and the firing rate falls despite continued stimulation
-high threshold respond to intense stimuli only but slow adapting and continue firing with continued stimulation
sense pain and temperature
activated by noxious mechanical and heat stimuli
Transmit sharp pain following injury
can be subdivided
- low threshold hence respond quickly in normal circumstances but rapidly adapt and the firing rate falls despite continued stimulation
-high threshold respond to intense stimuli only but slow adapting and continue firing with continued stimulation
what are c fibres?
- contrast to A fibres unmyelinated
. - tranmit pain, touch and temperature
-slow pain or second pain neurons
-poylmodeal or silent/chemoreceptive
- throbbing component to curtain stimuli
. - tranmit pain, touch and temperature
-slow pain or second pain neurons
-poylmodeal or silent/chemoreceptive
- throbbing component to curtain stimuli
what are A alpa fibres?
A beta fibres?
y fibres?
A beta fibres?
y fibres?
large motor, proprioreceptors
touch , small motor, ressure, modulation processing via gait theory
motor muscle spindels
touch , small motor, ressure, modulation processing via gait theory
motor muscle spindels
where can you find nocioreceptors?
do they have a free nerve ending?
do they have a free nerve ending?
superficial layer of skin
internal organs (lots of in periosteum, joint surfaces, falx ant tentorium of cranial vault, visercal organ less, so pain less localised)
yes
internal organs (lots of in periosteum, joint surfaces, falx ant tentorium of cranial vault, visercal organ less, so pain less localised)
yes
list the stimulators for nocireceptors
Stimulators
Bradykinin
Serotonin
Potassium
Histamine
Hydrogen ions
Bradykinin
Serotonin
Potassium
Histamine
Hydrogen ions
Inflammation resulting form tissue damage causes chemicals to be released and the influx of inflammatory cells. The result is an inflammatory soup of mediators including those that involve
activating
sensitising
recruiting (in the case of silent nociceptors)
nociceptors
This is via interactions on ion channels, receptor specific channels and by second messenger effects. What does that result in?
activating
sensitising
recruiting (in the case of silent nociceptors)
nociceptors
This is via interactions on ion channels, receptor specific channels and by second messenger effects. What does that result in?
-enhanced nociceptor excitability
-an altered response to a given stimulus
-Hyperalgesia - an increased response to a normally painful stimulus
-Nociceptors having an increased receptive field
This barrage of afferent information results in changes in the spinal cord
enhanced spinal nociceptor excitability - secondary hyperalgesia
-an altered response to a given stimulus
-Hyperalgesia - an increased response to a normally painful stimulus
-Nociceptors having an increased receptive field
This barrage of afferent information results in changes in the spinal cord
enhanced spinal nociceptor excitability - secondary hyperalgesia
what is neuropathic pain?
what is is caused by?
what is is caused by?
- spontaneous discharge
- ectopic discharge
- alteered channel expression (ion and g protein coupled recetors, receive the H and BK and PGE stuff)
- nerve sprouting ( axonal, dendritic iin periphery, fire off thier own and make new connections whch can be more sensitive
- nocireceptor sensitisation
damage to nervous system
- ectopic discharge
- alteered channel expression (ion and g protein coupled recetors, receive the H and BK and PGE stuff)
- nerve sprouting ( axonal, dendritic iin periphery, fire off thier own and make new connections whch can be more sensitive
- nocireceptor sensitisation
damage to nervous system
what does homeostasis mean?
Body’s ability to maintain internal stability (survival).
Failure to maintain homeostasis can result in pathological disease eg heart failure.
Failure to maintain homeostasis can result in pathological disease eg heart failure.
which bit of the brain does homeostasis regulate?
which part of this part does which in
supraoptic/paraventricular nuclei*
anterior/posterior hypothalamic nuclei
lateral hypothalamus*
arcuate/ventromedial nuclei /lateral hypothalamic area*
anterior/preoptic areas
suprachiasmatic nucleus
which part of this part does which in
supraoptic/paraventricular nuclei*
anterior/posterior hypothalamic nuclei
lateral hypothalamus*
arcuate/ventromedial nuclei /lateral hypothalamic area*
anterior/preoptic areas
suprachiasmatic nucleus
THE HYPOTHALAMUS major regulator of homeostasis
groups neurons regulate several important physiological functions
Water/electrolyte balance -supraoptic/paraventricular nuclei*
Temperature regulation -anterior/posterior hypothalamic nuclei
Thirst/drinking -lateral hypothalamus*
Hunger/satiety/regulating feeding behaviour -arcuate/ventromedial nuclei /lateral hypothalamic area*
Regulation sexual behaviour -anterior/preoptic areas
Regulation circadian rhythms -suprachiasmatic nucleus
how does the hypothalamus maintain homeostasis?
by affecting
Neuroendocrine (Posterior/Anterior pituitary)
Autonomic Nervous System (Sympathetic nervous system)
Neuroendocrine (Posterior/Anterior pituitary)
Autonomic Nervous System (Sympathetic nervous system)
what is homeostasis e.g. fluid regulation necessary for?
what two systems are maintained?
what two systems are maintained?
normal cellular metabolism
Maintenance of
-solute concentration (osmotic homeostasis)
-plasma volume (volume homeostasis)
Maintenance of
-solute concentration (osmotic homeostasis)
-plasma volume (volume homeostasis)
what do we understand under osmomtic regulation?
what is its major stimulus?
how does it regulate it?
what is its major stimulus?
how does it regulate it?
Body water gain -sodium ingestion eg foods
Increase plasma osmolality leads to cellular dehydration (water leaving cells by osmosis expands ECF)
Sodium load compared to water deprivation
Increase plasma osmolality leads to cellular dehydration (water leaving cells by osmosis expands ECF)
Sodium load compared to water deprivation
do does the regulatory process work at the osmotic homeostasis?
what does it result in? 4
what does it result in? 4
-Vasopressin (VP, antidiuretic hormone, ADH) secretion by magnocellular neurones of supraoptic nucleus (SON) & paraventricular nucleus of the hypothalamus (PVN)
-Specific stimulus (increase osmolality body fluid) increase secretion into blood stream;
-Circulating VP acts VP receptors (V2) kidney and
increase water permeability distal convoluted tubules (DCT) nephrons by insertion water channels into apical membrane tubular epithelial cells
- Increase water permeability collecting duct (CD)
Result
-Antidiuresis (conserve water)
-Movement water DCT & CD by OSMOSIS
-Decrease urine flow
-increase urine osmolality
-Specific stimulus (increase osmolality body fluid) increase secretion into blood stream;
-Circulating VP acts VP receptors (V2) kidney and
increase water permeability distal convoluted tubules (DCT) nephrons by insertion water channels into apical membrane tubular epithelial cells
- Increase water permeability collecting duct (CD)
Result
-Antidiuresis (conserve water)
-Movement water DCT & CD by OSMOSIS
-Decrease urine flow
-increase urine osmolality
How does change in blood osmolality initiate Vasopressin secretion from hypothalamus
Osmoreceptors in circumventricular organs
-vascular organ of the lamina terminalis (OVLT) senses osmolality
-Subfornical organ (SFO) near ianterior wall of 3V senses angiotension
the stimulation of vasopressin secretion has differnet pathways and involves different parts of the brain. name the pathways and the nuclei it involves.
median preoptic nucleus (MnPO)
Optic chiasm (OC)
Anterior commissure (AC)
There are three major pathways:
1 Osmoreceptors in OVLT sense the change, feedback to PVN or SON which simulates vasoprssion secretion into blood stream
2 OVLT stimulates MnPO via SON to PVN then stimulates vasopression
3 OVLT stimulate MnPO then stimulates SON and then drectly into blood stream without the PVN

Optic chiasm (OC)
Anterior commissure (AC)
There are three major pathways:
1 Osmoreceptors in OVLT sense the change, feedback to PVN or SON which simulates vasoprssion secretion into blood stream
2 OVLT stimulates MnPO via SON to PVN then stimulates vasopression
3 OVLT stimulate MnPO then stimulates SON and then drectly into blood stream without the PVN

how does angiotension stimulate the osmotic response of the brain? to which centeres doesit go to stimulate vasopression?
Angiotensin stimulates the subforinal organ which then has various pathways:
1 It can go to the median preoptic nucleus and from there stimulate the PVN or SON which then stimulate the secreition of vasopressin into the blood stream
2 It can to directly tothe PVN or SON and release vasopression

1 It can go to the median preoptic nucleus and from there stimulate the PVN or SON which then stimulate the secreition of vasopressin into the blood stream
2 It can to directly tothe PVN or SON and release vasopression

there is body fluid homeostasis but also a metabolic homeostasis which comprises a short term and a long term central control of feeding. explain the short term control of feeding behaviour.
Motivation to eat
- timing last meal
-appeal food on offer
Feeding ends several satiety signals
-gastric distension
- cholecystokinin (CCK)
-insulin
-> in response to gastric distention
- timing last meal
-appeal food on offer
Feeding ends several satiety signals
-gastric distension
- cholecystokinin (CCK)
-insulin
-> in response to gastric distention
what is the long term control of metabolic homeostasis concerning the long term control?
-Leptin levels high with food intake
-released blood stream adipocytes and stimulates hypothalamus
- Activation leptin receptors on Arcuate Nucleus (ARH) neurones
- ARH neurones responding rise leptin contain peptide neurotransmitters (needed to stimulate arcurate nucleus)
alpha-melanocyte-stimulating hormone (αMSH)
cocaine-and amphetamine-regulated transcript (CART)
-released blood stream adipocytes and stimulates hypothalamus
- Activation leptin receptors on Arcuate Nucleus (ARH) neurones
- ARH neurones responding rise leptin contain peptide neurotransmitters (needed to stimulate arcurate nucleus)
alpha-melanocyte-stimulating hormone (αMSH)
cocaine-and amphetamine-regulated transcript (CART)
what are the three responses to excessive adiposity of the body?
Humoral response
Thyroid stimulating hormone (TSH) & adrenocorticotropic hormone (ACTH) from pituitary act on thyroid & adrenal glands raise metabolic rate cells throughout body
Visceromotor Response (sympathetic response)
tone sympathetic nervous system raise metabolic rate by raising body temperature
Somatic Response
decrease feeding behaviour
Activation of αMSH & CART neurones within arcuate nucleus (ARH) orchestrate this integrated response
Thyroid stimulating hormone (TSH) & adrenocorticotropic hormone (ACTH) from pituitary act on thyroid & adrenal glands raise metabolic rate cells throughout body
Visceromotor Response (sympathetic response)
tone sympathetic nervous system raise metabolic rate by raising body temperature
Somatic Response
decrease feeding behaviour
Activation of αMSH & CART neurones within arcuate nucleus (ARH) orchestrate this integrated response
explain the humoral response in more detail ( of the metabolic homeostasis in reponse to increased leptin levels)
Humoral response
- Leptin stimulates the αMSH/CART neurones in ARH
- These neurones stimulate the PVN to release the hypophysiotropic hormones TSH/ACTH into the circulation to act on thyroid and adrenal glands to raise metabolic rate in body

- Leptin stimulates the αMSH/CART neurones in ARH
- These neurones stimulate the PVN to release the hypophysiotropic hormones TSH/ACTH into the circulation to act on thyroid and adrenal glands to raise metabolic rate in body

explain the ciscero motor response in homeostasis (metabolic) to an increased level in leptin.
Leptin stimulates the αMSH/CART neurones in ARH
PVN medulla + SPN
end organ for an increase in sympathetic nerve activity
- αMSH/CART medulla + SPN end organ for an increase in sympathetic nerve activity
explain the somatic response in metabolic homeostasis to an elevated leptin level.
Somatic motor response
αMSH/CART lateral hypothalamic area (LHA)
Inhibit feeding
αMSH/CART lateral hypothalamic area (LHA)
Inhibit feeding
what happens if leptin in blood is decreased, how does the homeostatic metabolic thing react?
- Decrease leptin turn off αMSH & CART responses
-results in activation of sub group neurones in ARH that contain neuropeptides
neuropeptide Y (NPY)
agouti-related peptide (AgRP)
These neurones connected PVN & LHA
-NPY & AgRP inhibit TSH & ACTH secretion (decrease vicero-motor response)
-Activate parasympathetic nervous system (inhibit sympathetic nervous system)
-Stimulate feeding behaviour via LHA
- LHA neurones contain melanin-concentrating hormone (MCH) and orexin neurons which initiate feeding behavior
-results in activation of sub group neurones in ARH that contain neuropeptides
neuropeptide Y (NPY)
agouti-related peptide (AgRP)
These neurones connected PVN & LHA
-NPY & AgRP inhibit TSH & ACTH secretion (decrease vicero-motor response)
-Activate parasympathetic nervous system (inhibit sympathetic nervous system)
-Stimulate feeding behaviour via LHA
- LHA neurones contain melanin-concentrating hormone (MCH) and orexin neurons which initiate feeding behavior
explain the Control of feeding by lateral hypothalamic peptides.
-One group of LHA neurones contain melanin-concentrating hormone (MCH)
-MCH receive input from leptin sensitive cells (αMSH/CART) of ACH
-MCH containing neurones connections throughout brain
-monosynaptic innervation mostly to cortex
-Cortex organise/initiates goal-directed behaviours (raiding fridge/drinking more beer)
-MCH cells inform cortex levels leptin, may contribute significantly to motivating the search for food
- alsok LHA neurones contain peptide OREXIN that project to cortex
-Orexin neurones receive direct innervation from ARH
-Orexin stimulating feeding behaviour
-Stimulate MCH & Orexin neurones when leptin levels fall in blood
Inhibit MCH & Orexin neurones when leptin levels increase in blood
Orexin role control sleep links to narcolepsy.
-MCH receive input from leptin sensitive cells (αMSH/CART) of ACH
-MCH containing neurones connections throughout brain
-monosynaptic innervation mostly to cortex
-Cortex organise/initiates goal-directed behaviours (raiding fridge/drinking more beer)
-MCH cells inform cortex levels leptin, may contribute significantly to motivating the search for food
- alsok LHA neurones contain peptide OREXIN that project to cortex
-Orexin neurones receive direct innervation from ARH
-Orexin stimulating feeding behaviour
-Stimulate MCH & Orexin neurones when leptin levels fall in blood
Inhibit MCH & Orexin neurones when leptin levels increase in blood
Orexin role control sleep links to narcolepsy.
what is dysphasia?
What is dysarthria?
What is dysarthria?
Dysphasia (one in a group of speech disorders in which there is impairment of the power of expression by speech, writing, or signs, or impairment of the power of comprehension of spoken or written language. More severe forms of dysphasia are called aphasia.
dysarthria (motor speech disorder resulting from neurological injury, characterized by poor articulation
dysarthria (motor speech disorder resulting from neurological injury, characterized by poor articulation
what is the occulo-cehpahic refelx?
also called dolls eyes
If dolls eyes are intact, they stay fixed on a point while moving the head (good). If dolls eyes are absend they move with head
If dolls eyes are intact, they stay fixed on a point while moving the head (good). If dolls eyes are absend they move with head
what are the brainstem functions? 7
Arousal/consciousness
Respiratory drive
Maintenance of blood pressure
All motor inputs
All sensory inputs (except olfaction/vision)
Autonomic efferents pass through it
Cranial nerve reflexes easily testable
Respiratory drive
Maintenance of blood pressure
All motor inputs
All sensory inputs (except olfaction/vision)
Autonomic efferents pass through it
Cranial nerve reflexes easily testable
what tests are there for brain stem death?
• confirmation of absent brainstem reflexes
- pupillary response (unresponsive pupils)
- corneal reflex (Stimulate the cornea with cotton wool, eyes dont blink if bad)
-motor responses within cranial nerve distributions
- gag reflex, cough reflex (Gag reflex stimulate pharynx with tongue depressor, Cough reflex stimulate carina with suction catheter, both stimulate cranial nerve nine and ten)
- vestibulo-ocular reflex (Look insight the ear, if bleed form ear then skull fracture. Then put in ice water. Normally you thinkg you would fall olver and move the eyes dowards the cold warter comign in. If intact, you move the eyes around and look around since you think you are fallling over. )
• confirmation of persistent apnoea (pre-oxygenate with 100% O2 for 10 minutes, and allow PaCO2 to rise to 5kPa; disconnect patient from ventilator while maintaining
adequate oxygenation and allow PaCO2 to rise above 6.65kPa; confirm no spontaneous
respiration and reconnect ventilator –> rapid breathing lowers CO2).
Tags: -
Quelle:
Quelle:



